COVID-19 vaccines have been free and broadly available to adults in all states and the District of Columbia since mid-April 2021, meaning adults in the U.S. have generally been able to be fully vaccinated for COVID-19 since late May 2021 if receiving a two-dose vaccine. COVID-19 vaccines are highly effective at preventing severe disease, hospitalization, and death from COVID-19.
Despite the availability of safe and effective COVID-19 vaccines, vaccination rates have lagged, particularly in some states and among younger people. As of early December 2021, 17% of adults over the age of 18 in the U.S. remain unvaccinated for COVID-19. These COVID-19 hospitalizations are devastating for patients, their families, and health care providers. The hospitalizations are also costing taxpayer-funded public insurance programs and the workers and businesses paying health insurance premiums. Our recent analysis found that insurers are beginning to reinstate cost-sharing for COVID-19 treatment, though patients still only pay a small share of the total costs.
In this analysis, we seek to quantify the number of hospitalizations that could have been prevented by vaccination and the total cost of these hospitalizations. We find there were a total of 690,000 vaccine-preventable COVID-19 hospitalizations from June through November 2021. These hospitalizations correspond with the Delta variant surge. (There is still uncertainty around the vaccine’s effectiveness at preventing hospitalizations resulting from the Omicron variant taking hold in December, though early indications suggest vaccination will be protective against severe disease.)
While real-time data on the cost of all COVID-19 hospitalizations are not publicly available, various sources point to an average hospitalization cost of around $20,000. The Centers for Medicare and Medicaid Services (CMS) reports that Medicare fee-for-service COVID-19 hospitalizations average $24,033. Another study of Medicare fee-for-service enrollees found an average COVID-19 hospitalization cost $21,752. A FAIR Health analysis of private claims data including employer and private Medicare Advantage plans found that median in-network COVID-19 hospitalization costs ranged from $17,094 for people over age 70 to $24,012 for people in their 50s. Similarly, our analysis of pre-pandemic private insurance claims for pneumonia hospitalizations with complications averaged $20,292 (though the cost for hospitalizations requiring a ventilator are much higher).
If each of these preventable hospitalizations cost roughly $20,000, on average, that would mean these largely avoidable hospitalizations have already cost billions of dollars since the beginning of June.
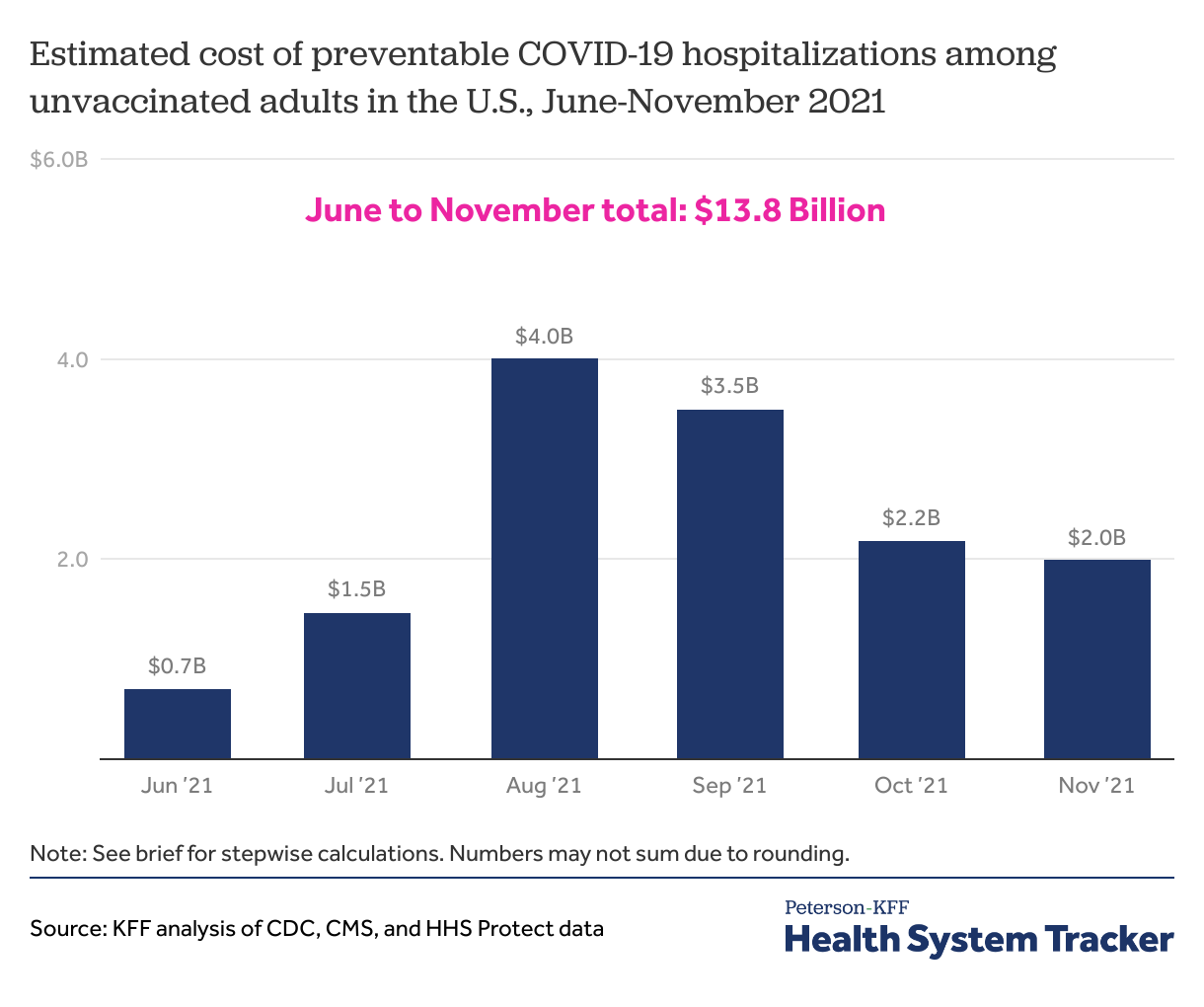
From June through November 2021, preventable COVID-19 hospitalizations among unvaccinated adults cost over $13 Billion
Based on our estimates, described below, we find preventable COVID-19 cost $13.8 Billion from June to November in 2021.
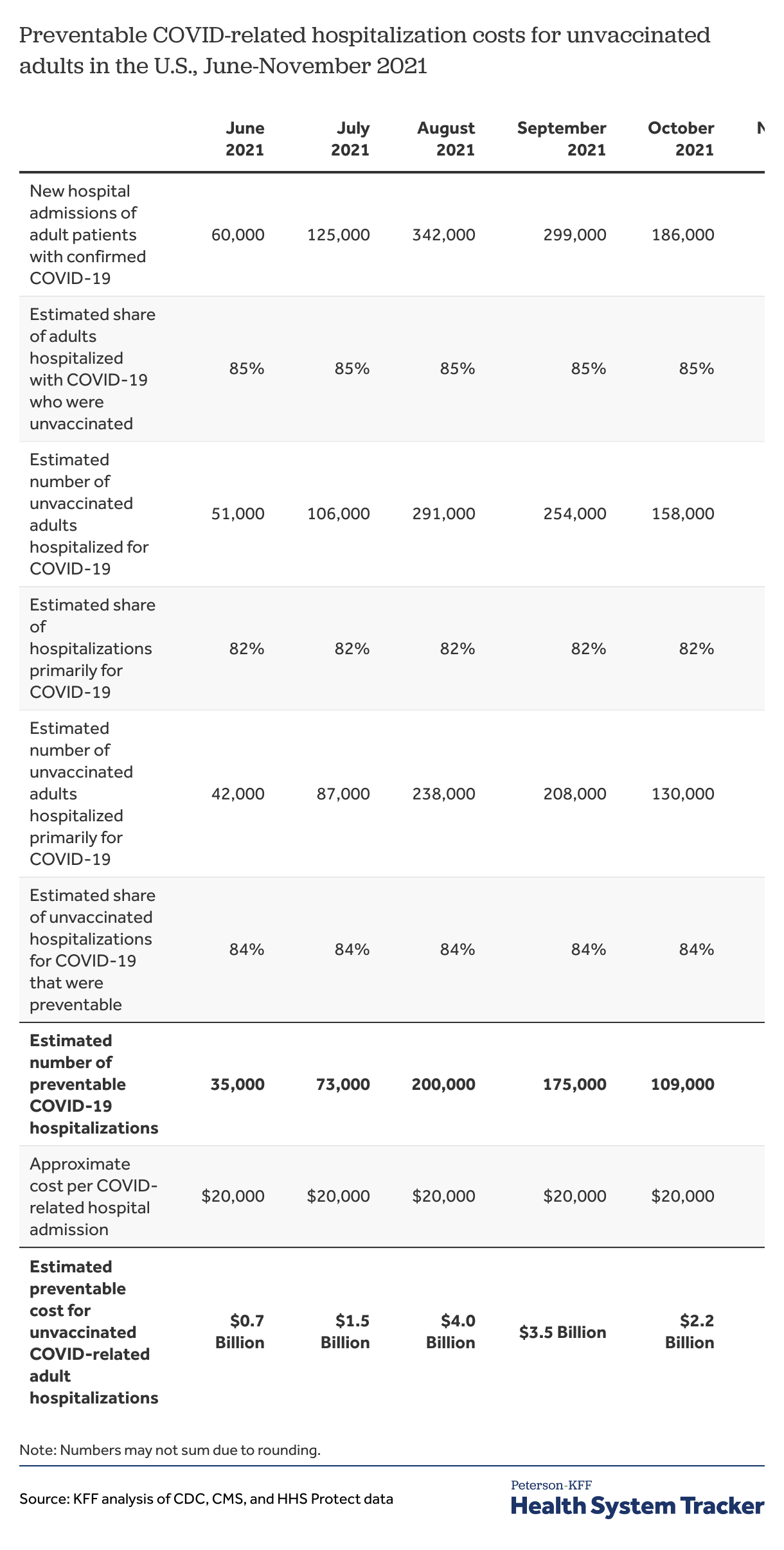
We used counts of adult hospitalizations with confirmed COVID-19 in recent months reported to HHS to estimate preventable hospitalization costs for unvaccinated adults. We focus on hospitalizations of adults (ages 18+) with COVID-19 because many children are still ineligible for the COVID-19 vaccine, and even those minors who are eligible may need parental consent to get the vaccine.
Over 690,000 COVID-19 hospitalizations could have been prevented by vaccination between June to November 2021
To estimate the number of preventable hospitalizations, our first step is to remove vaccinated adults from the number of people hospitalized with COVID-19. Doing so gives us the number of adults hospitalized with COVID-19 who are unvaccinated. Based on the number of breakthrough hospitalizations (hospitalizations among those who are fully vaccinated with a COVID-19 diagnosis) reported to the CDC, we estimate that 98.6% of people hospitalized with a COVID-19 diagnosis between June and August 2021 were unvaccinated. Although the number of vaccinated people hospitalized for COVID-19 increased in August, the number of unvaccinated people hospitalized for COVID-19 also increased, meaning that unvaccinated people still represent a similar share of total hospitalizations. A recent CDC study found in the period after the Delta variant became dominant (June 20 – July 17), fully vaccinated people accounted for 14% of hospitalizations in 13 U.S. jurisdictions. Our analysis with Epic Research similarly found fully vaccinated people accounted for 15% of COVID-19 hospitalizations from June-September 2021. Though these estimates may not be generalizable to the U.S. population, it is a more conservative estimate of the share of COVID-19 hospitalizations among vaccinated people. Therefore, we multiply the number of adults hospitalized with COVID-19 by 85% to get the number of unvaccinated adults hospitalized with COVID-19.
Our second step is to focus on the hospitalizations that are primarily for COVID-19 treatment. Although these unvaccinated people were hospitalized with a confirmed COVID-19 diagnosis, COVID-19 may not have been their primary reason for being hospitalized. Some people may have been hospitalized for other conditions or comorbidities that would have caused them to be hospitalized even if they had not been diagnosed with COVID-19. Data reported by CDC for vaccinated patients through August 30, 2021 showed 75% of hospitalizations with COVID-19 diagnosis were primarily for COVID-19. Unvaccinated people have a higher risk of severe illness from a COVID-19 infection than vaccinated people. Our analysis with Epic Research found 82% of unvaccinated patients hospitalized with COVID-19 had COVID-related complications or treatment, whereas 72% of fully vaccinated patients hospitalized with COVID had COVID-related complications or treatment. We multiplied the number of unvaccinated adults hospitalized by 82% to arrive at the number of unvaccinated adults hospitalized primarily because of COVID-19.
Our third step is to adjust for the fact that – even if these unvaccinated adults had gotten the vaccine, the vaccine would not prevent 100% of hospitalizations. Based on CDC data for the effectiveness of the COVID-19 vaccines in preventing hospitalizations at 13-24 weeks, we assume that 84% of hospitalizations primarily for COVID-19 are preventable with vaccinations. Multiplying the number of adults hospitalized primarily due to COVID-19 by the percent of hospitalizations preventable by vaccination (84%) gives us the number of preventable hospitalizations. This is again a conservative assumption, as other studies have pointed to a higher level of protection from hospitalization.
Our final step is to multiply the number of preventable hospitalizations times the cost of each hospitalization. As described above, we use a typical cost of $20,000 for a hospital admission for COVID-19 based on prior studies of similar admissions, but this has many limitations and is only meant to be illustrative. For example, we do not know the payer mix for COVID-19 hospitalizations among the non-elderly, nor do we know the typical hospitalization cost for Medicaid patients (although there is reason to believe it is in the same ballpark). Additionally, while we know that hospital prices vary greatly geographically and that COVID-19 hospitalizations are more concentrated in certain parts of the U.S., we do not attempt to adjust for geographic differences in price or volume.
Still, this ballpark figure is likely an understatement of the cost burden from preventable treatment of COVID-19 among unvaccinated adults. First, we do not include the cost of outpatient treatment, which is likely substantial. A Medicare study found patients with COVID-related admissions had multiple outpatient visits (3.2 on average) that cost approximately $164 each (and this is only for those COVID-19 patients who were hospitalized at one point). In our analysis of pre-pandemic private insurance claims, we estimated a typical outpatient office visit costs $105 on average. An analysis of privately insured noted COVID-19 outpatient treatment costs can average $500-$1,000 per patient. Second, there is reason to believe average costs for COVID-19 hospitalizations may be even higher than $20,000 based on other studies of privately insured and Medicare. One study that has not yet been peer reviewed found that while the median hospitalization costs private payers $25,339, the mean cost was $42,200. Similarly, in their justification for charging higher premiums to unvaccinated employees, Delta Airlines said their average hospitalization cost was $50,000 (though it is unclear if this is the median or mean cost).
Additionally, although breakthrough infections and hospitalizations are rare, unvaccinated people are also more likely to spread the virus to those who have taken measures to protect themselves and others, and those costs are not included in these estimates.
Implications of avoidable COVID-19 hospitalization costs among unvaccinated people
The monetary cost of treating unvaccinated people for COVID-19 is borne not only by patients but also by society more broadly, including taxpayer-funded public programs and private insurance premiums paid by workers, businesses, and individual purchasers.
Only a small share of the cost of a COVID-19 hospitalization is paid directly by patients themselves. In our analysis of privately insured patients hospitalized with pneumonia, the typical out-of-pocket payment was about $1,300. Out-of-pocket costs may be higher for people based on their health insurance plan and how the COVID-19 hospitalization costs are billed. That is a significant amount for most patients to pay, but it is far less than the amount covered by public and private insurance coverage.
The Affordable Care Act and other laws prohibit insurers from charging unvaccinated people higher premiums. Though through wellness programs, employers could impose higher costs. Private insurers have begun reinstating cost-sharing for COVID-19 hospitalizations. The federal government requires insurers to cover the cost of COVID-19 tests without cost sharing for individualized diagnosis purposes but insurers are not required to cover the cost of COVID-19 testing for employment purposes. Unvaccinated workers may be required to get COVID-19 tests regularly to physically return to work, and insurers may shift some or all costs for those tests to the workers. Adults can largely avoid these out-of-pocket costs and severe illness by getting the free vaccine.
Though there was of course a societal cost to develop and distribute vaccinations, the vaccines save the U.S. health system money in the longer run by preventing costly hospitalizations. (Although the cost of treating COVID-19 patients has an upward effect on health spending and premiums, overall health services utilization and spending have been suppressed during the pandemic due to stay-at-home measures, potential risk of COVID-19 infection at a hospital or doctors’ offices, and concerns over hospital capacity). In addition to preventable direct monetary costs for treatment of unvaccinated people, re-opening of schools and economic recovery also suffers as increasing COVID-19 cases continue to put Americans at risk of avoidable severe illness and even death.
Methods
We used Department of Health and Human Services (HHS) data for estimates of new adult hospital admissions with confirmed COVID-19. We summed the previous day adult patient admissions across all days in each month (using variable: previous_day_admission_adult_covid_confirmed).
We used CDC data on hospitalizations reported among people with COVID-19 vaccines for breakthrough hospitalizations to estimate the share of hospitalizations with a COVID-19 diagnosis that were among unvaccinated adults. From June 1-August 30, 2021, CDC reported 7,617 patients with COVID-19 breakthrough infections were hospitalized and about 25% of those breakthrough hospitalizations were asymptomatic or admitted for a reason unrelated to COVID-19. Based on approximately 530,000 hospital admissions with confirmed COVID-19 diagnosis in June-August 2021, we estimate 98.6% of hospital admissions with COVID-19 during this period were among unvaccinated people (1 – 7,617/530,000 equals 98.6%). Reports of COVID-related hospitalizations among unvaccinated people range from 95% to 99.9% by state. We used the estimate from our analysis with Epic Research that found unvaccinated people accounted for 85% of COVID-19 hospitalizations from June-September 2021. Additionally, our assumption on the share of COVID-19 hospitalizations among unvaccinated adults that were COVID-related is based on our analysis with Epic Research, which found 82% of unvaccinated patients hospitalized with COVID-19 had COVID-related complications or treatment.
We based our assumption of the number preventable hospitalizations with COVID-19 vaccines on recent CDC MMWR studies of COVID-19 vaccine effectiveness against hospitalizations among people who received 2 doses of an mRNA vaccine. Although another recent CDC MMWR study of New Yorkers reported a higher COVID-19 vaccine effectiveness against hospitalizations, we use the lower estimate as a conservative assumption.
The Peterson Center on Healthcare and KFF are partnering to monitor how well the U.S. healthcare system is performing in terms of quality and cost.