Researchers have used a variety of measures to assess the impact of the COVID-19 pandemic, including deaths directly attributed to COVID-19 infection and deaths in excess of prior years’ death rates. However, these measures do not incorporate the prematurity of deaths or differences in age at death between countries. While the elderly have been at the highest risk of becoming seriously ill due to COVID-19 infections, COVID-19 also affected mortality rates among younger individuals.
In this brief, we review excess death rates in the U.S. and peer countries by age groups to examine how the pandemic has affected excess mortality rate among younger people. We look specifically at the excess deaths that arose in 2020 to examine how the age at death during the pandemic has differed between the U.S. and peer nations. We also estimate the excess potential years of life lost (a measure of “premature excess death”) during the pandemic, and explore racial disparities in the age of death in the U.S.
We find that, among similarly large and wealthy countries, the U.S. had among the highest excess mortality rates in 2020, and younger people were more likely to have died due to the pandemic in the U.S. than younger people in other countries. With a much higher rate of death among people under age 75, the U.S. had the highest increase in premature deaths due the pandemic in 2020. Before the pandemic, the U.S. already had the highest premature death rate of peer nations, by far. We find that per capita premature excess death rate in the U.S. was over twice as high as the next closest peer country, the U.K. The higher rate of new premature deaths in the U.S. compared to peer countries was driven in part by racial disparities within the U.S. Looking at age differences in excess mortality by race, we find that American Indian and Alaska Native (AIAN), Hispanic, Black, and Native Hawaiian and Other Pacific Islander (NHOPI) people in the U.S. were more likely to have died at younger ages during the pandemic in 2020 than non-elderly White or Asian adults in the U.S.
During the pandemic, the U.S. lost an additional 3.6 million potential years of life in 2020. Among excess deaths in 2020, the average person lost 14 years in the U.S. compared to an average of 8 years in peer countries before the age of 75. Excess mortality rates were higher among younger people of color, in part, leading to higher premature excess deaths among people of color in the U.S. Of the potential years of life lost in the U.S., 30% were among Black people and another 31% were among Hispanic people, compared to their share of the U.S. population at 12.2% and 18.5%, respectively. Although discussions in the U.S. of how to mitigate the continued impact of COVID-19 have often pegged the economy against deaths among the elderly, the pandemic has also led to high excess mortality rates among younger people, including working age adults.
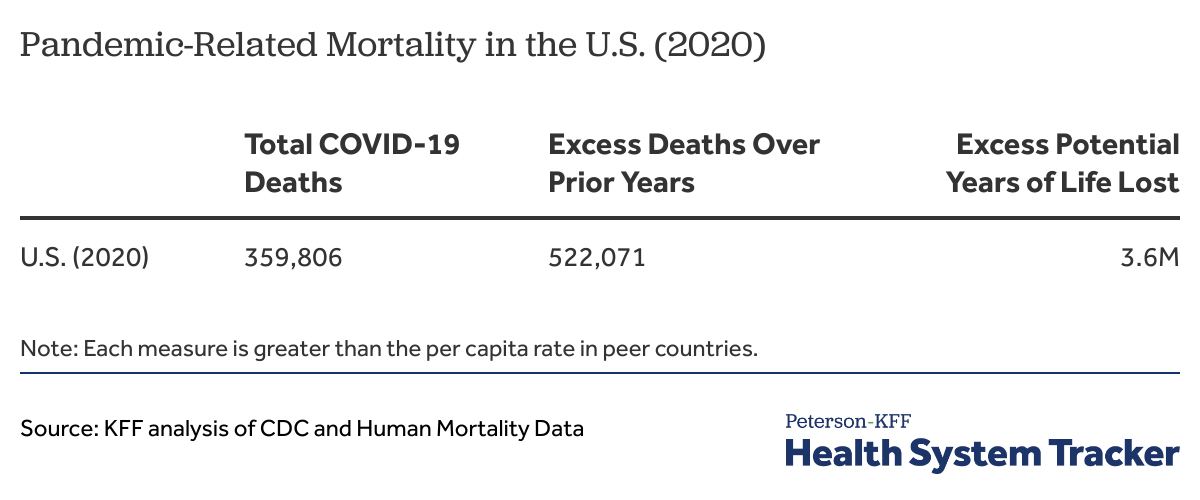
In 2020, the U.S. had the highest pandemic-related mortality and potential years of life lost among peer countries
Excess deaths by age groups in the U.S. and peer countries during the pandemic
People over the age of 65 are at particularly high risk of serious complications and death arising from COVID-19 infection, but COVID-19 was also a leading cause of death among younger people in the U.S. During the pandemic, we find that the U.S. saw the largest per capita increase in deaths among younger (non-elderly) people, among similarly large and wealthy nations in 2020.
“Excess deaths” represent the number of deaths beyond what is expected in a typical year. This measure illustrates the mortality directly or indirectly associated with the COVID-19 pandemic.
The U.S. had the highest increase in mortality rate among non-elderly people due to the pandemic among peer countries in 2020
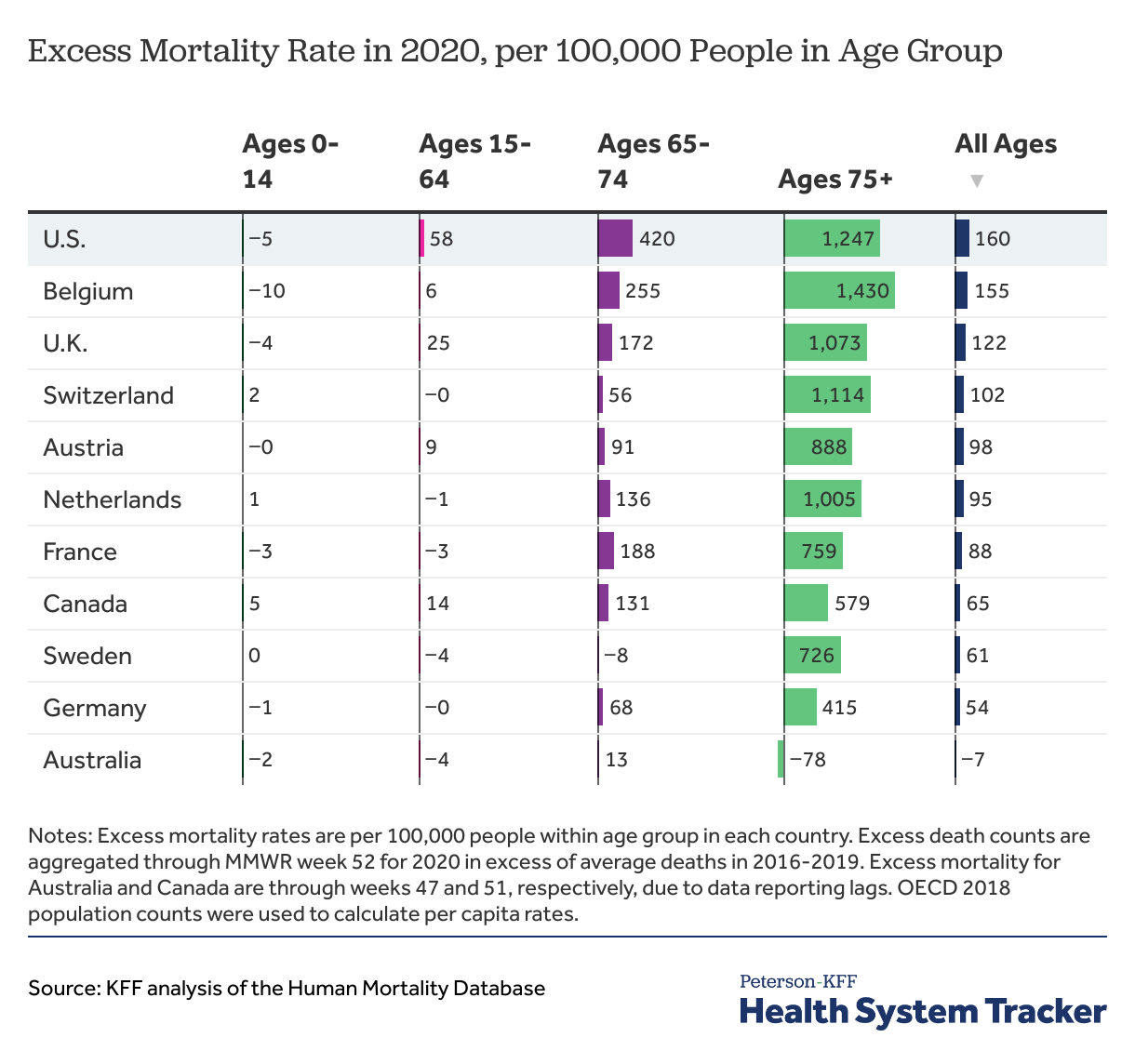
To compare excess deaths between the U.S. and peer countries, we analyzed the Human Mortality Data for deaths in 2020 over the average deaths in a typical year. Among peer countries, the U.S. had the highest overall excess mortality rate in 2020 with 160 excess deaths per 100,000 people across all ages. Belgium was only slightly behind with 155 excess deaths per 100,000 people across all ages. The U.K. had the third highest excess mortality rate in 2020 with 122 excess deaths per 100,000 people in 2020 across all ages. In one peer country (Australia) that had a low incidence of COVID-19 deaths, the excess mortality rate in 2020 even fell across all ages. The Human Mortality Database did not include data on Japan, but according to other analyses, excess mortality rate also fell in Japan in 2020.
The U.S. had by far the highest excess mortality rate among younger people under age 75 in 2020. Although Belgium was only slightly behind the U.S. in overall excess mortality, most of the excess deaths in Belgium were among the elderly, particularly ages 75 and older. Almost half (48%) of excess deaths in the U.S. were among people younger than 75 years, whereas only 18% of excess deaths in Belgium were among people younger than 75. The excess mortality rate per 100,000 people in the age group was almost 10 times higher among people ages 15-64 in the U.S. than in Belgium and 68% higher among people ages 65-74 in the U.S. than in Belgium.
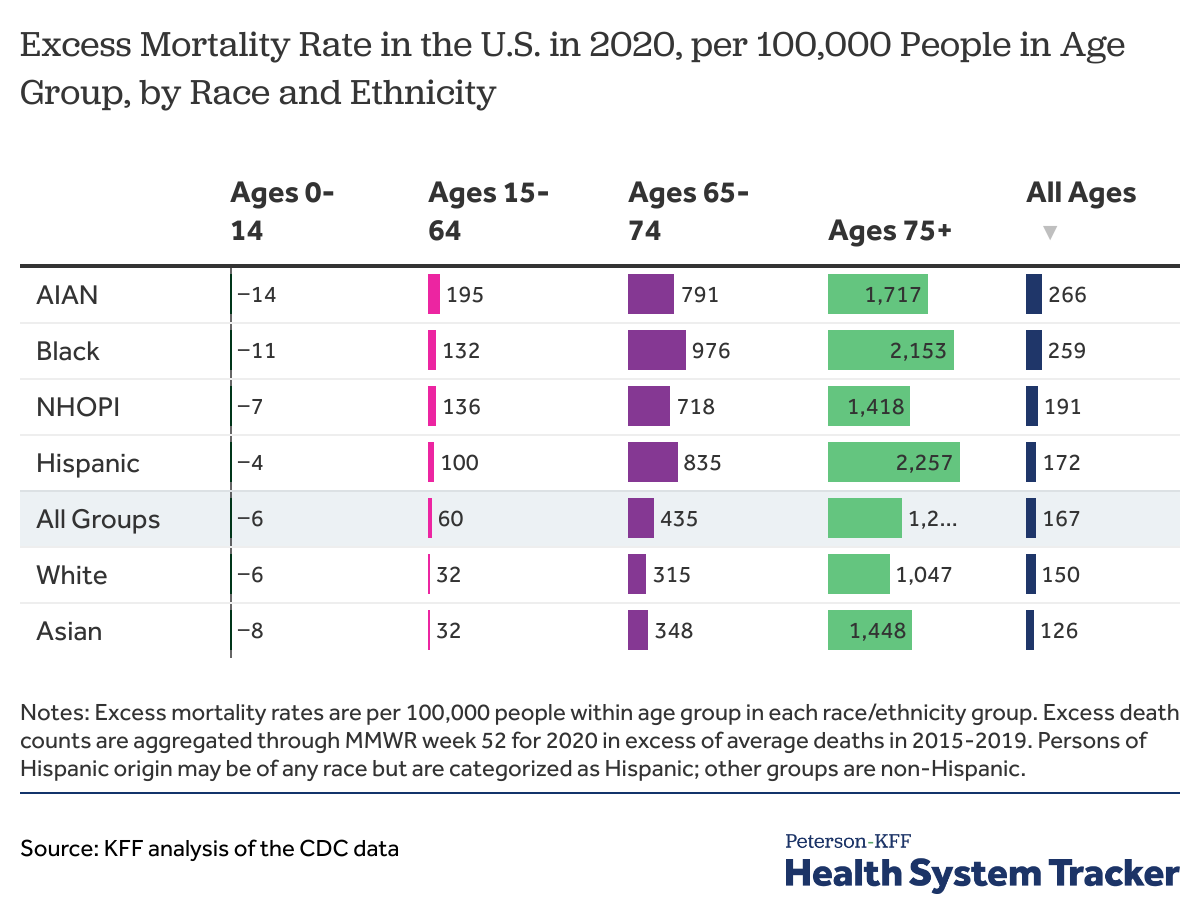
Higher excess deaths among younger people in the U.S. were partly due to racial disparities
We evaluated racial disparities in excess mortality by age groups using CDC excess death data comparing deaths in 2020 over average deaths in 2015-2019. Excess mortality rates among younger people were higher for American Indian and Alaska Native (AIAN), Native Hawaiian and Other Pacific Islander (NHOPI), Black, and Hispanic people than for other groups. Among AIAN people ages 15-64, excess deaths were 195 per capita in 2020, which is 44% higher than the excess mortality rate in the next closest group, NHOPI people ages 15-64, with 136 excess deaths per 100,000 people. Excess mortality rate in the 65-74 age group was the highest for Black people (976 excess deaths per capita), followed by Hispanic people (835 excess deaths per capita). Mortality rates among the elderly ages over 75 were higher among Hispanic, Black, AIAN, Asian, and NHOPI people compared to White people in the U.S.
Causes of excess mortality
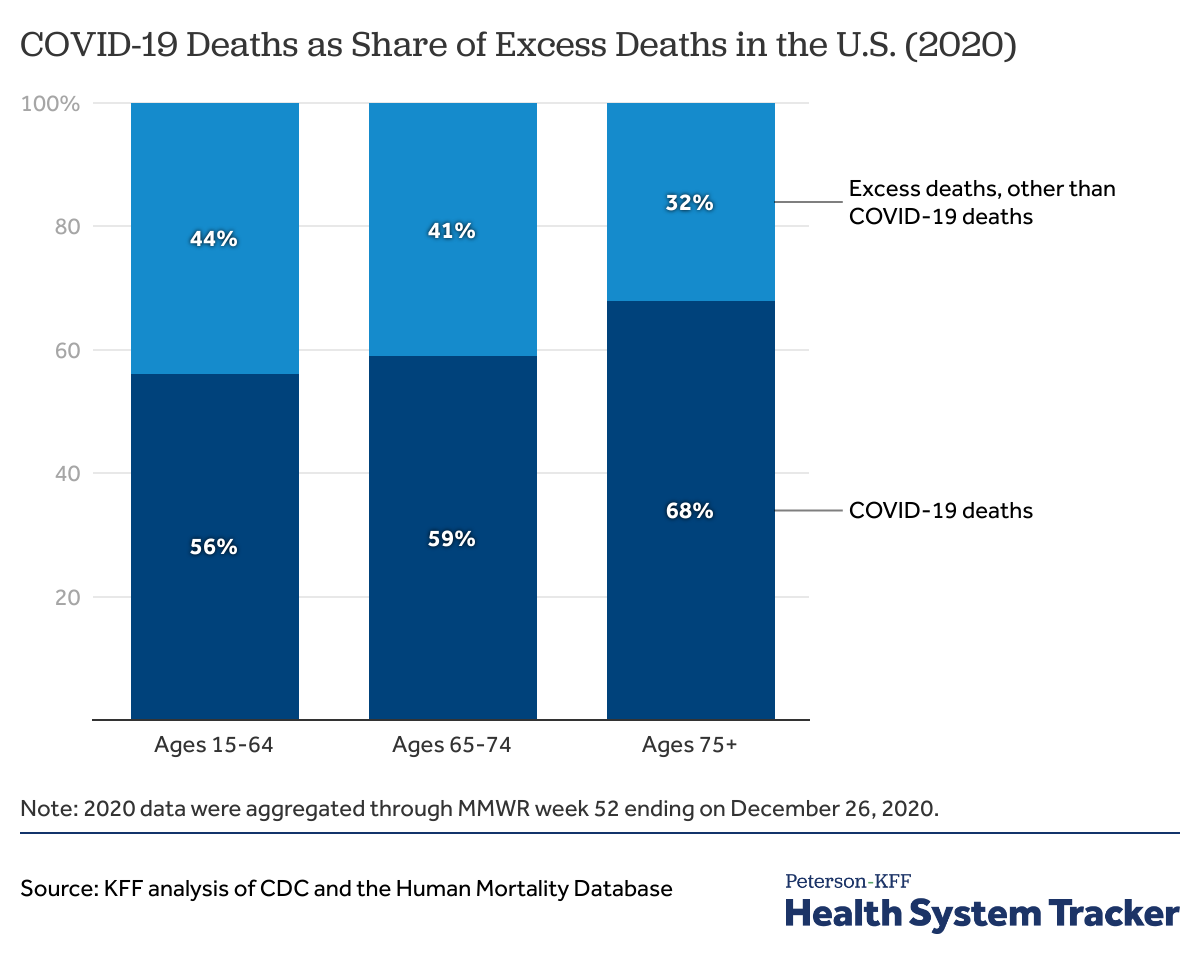
The high excess death rate among non-elderly people in the U.S. is likely due to direct and indirect deaths caused by COVID-19. We compared CDC reported COVID-19 deaths to the total excess deaths based on the Human Mortality Database by age groups in the U.S. in 2020.
COVID-19 deaths accounted for a majority of excess deaths among younger and elderly people in 2020 in the U.S.
Deaths directly attributed to COVID-19 accounted for two thirds of excess deaths in the U.S. in 2020. COVID-19 deaths as a share of excess deaths are lower among younger age groups. Nonetheless, COVID-19 is attributed for a majority of excess deaths among ages 15-64 (56%) and ages 65-74 (59%). There is reason to suspect that many of the excess deaths not directly attributed to COVID-19 could still have been caused by COVID-19 infection (due to inadequate testing, particularly early in the pandemic). This suggests the true toll of the pandemic might be undercounted in the COVID-19 mortality rates by a large margin. CDC has stated that the death count from causes that could be related to COVID-19 infections have also increased in 2020 (such as heart diseases, strokes, and Alzheimer’s disease and dementia). Additionally, CDC data shows deaths due to other causes also increased in 2020, including due to increased overdose fatalities. So, the difference between the excess deaths and the deaths attributed to COVID-19 might be because of an undercount of COVID-19 deaths, and the indirect impact of the pandemic leading to additional fatalities, including due to delayed or foregone care.
Excess potential years of life lost during the pandemic in the U.S. and peer countries
“Potential years of life lost” measures premature deaths and is used to compare differences in disease burden and longevity across countries. This measure is calculated by summing the years of life up to a limit of life expectancy from the age at death. To compare the extent of premature deaths in the U.S. and peer nations, we calculated the potential years of life lost up to age 75 using excess deaths during 2020 (the deaths beyond those expected in a normal year). In this analysis we follow the methods of the OECD, which recently began using 75 years as the age limit in calculation of potential years of life lost. Although excess deaths over age of 75 in 2020 were also premature compared to a typical year, they are not included in the potential years of life lost calculation as defined by the OECD.
The U.S. already had the highest premature death rate before the pandemic. Here, we look at premature deaths in excess of those in a typical year, which we refer to as premature “excess” deaths, or “excess” potential years of life lost. The premature excess death rate shows the number of excess potential life years per capita that may be lost due to the COVID-19 pandemic over a typical year and indicates a rise in premature death in 2020. The number of excess potential years of life lost increased in the U.S. more than in other countries in 2020, which means the COVID-19 pandemic has widened the gap between the U.S. and peer countries in premature deaths.
We calculate excess potential years of life lost using the number of excess deaths from the Human Mortality Database up to the age limit of 75. As an illustration, each excess death in the 65-74 age group is counted as losing 5.5 potential years of life (75 age limit minus 69.5 equals 5.5 years). U.S. Centers for Disease Control and Prevention (CDC) data show that weighted average excess death age in the 15-64 age group is 50 years. Because more granular age at death data were not available in all countries, we used an age of 50 (based on data in the U.S.) to calculate excess potential years of life lost to the age limit of 75 for the 15-64 age group for all countries. This decision is conservative and might make the gap between the U.S. and other countries appear smaller than it is, because 50 years of age is likely lower than the average age at death in the 15-64 age group in comparison countries. As a final step, we summed excess potential years of life lost across ages 0-74 for excess potential years of life lost in each nation. For comparison across countries, the premature excess death rates were calculated per 100,000 people within each age group in each country.
The U.S. had the highest excess potential years of life lost per capita in 2020 among peer countries
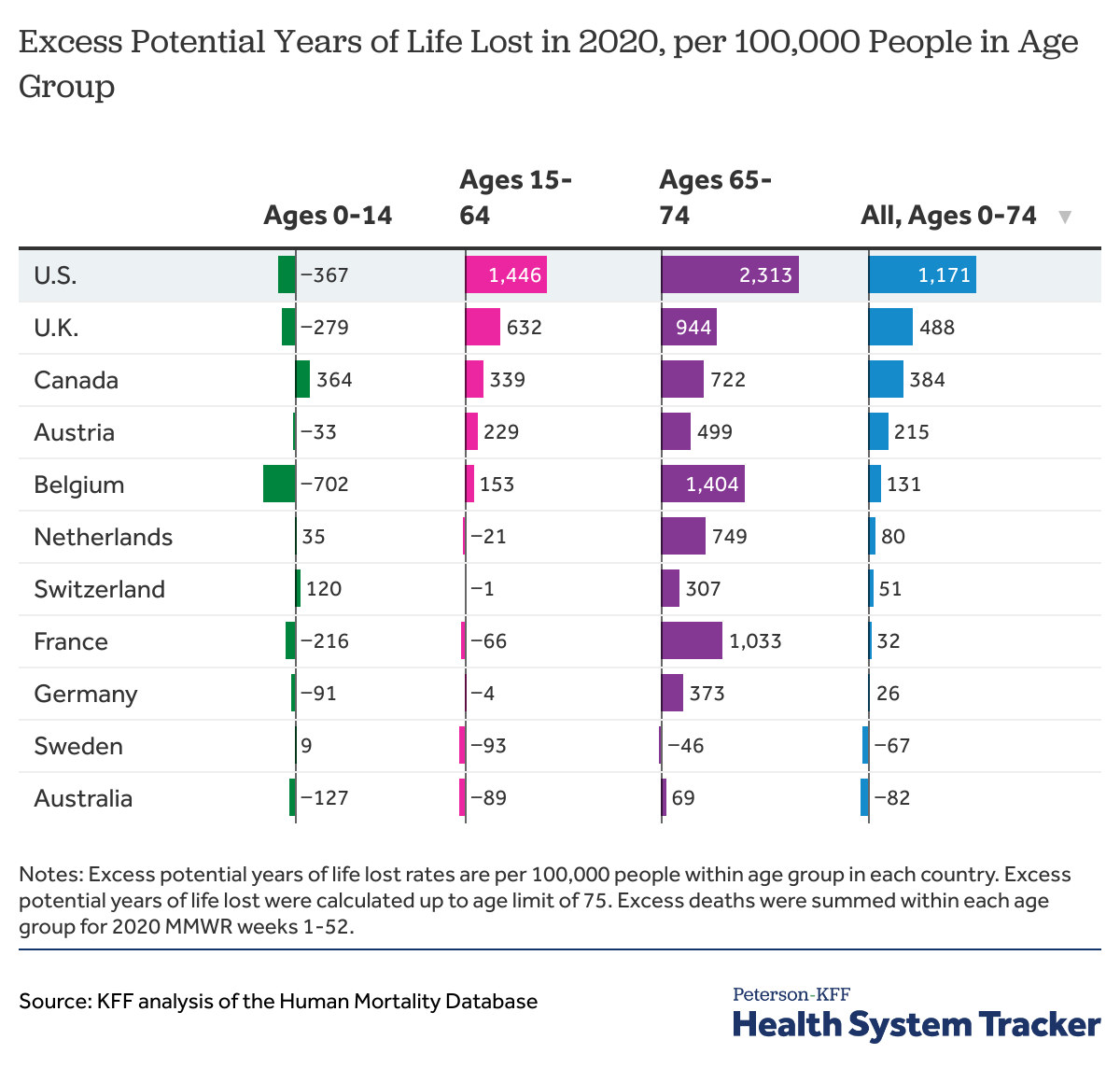
The U.S. had the highest premature excess death rate per capita among peer countries in 2020 across all ages. We find that more young (non-elderly) people died in the U.S. than in a typical year and at a higher per capita rate than in peer countries. Based on the Human Mortality Database, the U.S. had 1,171 excess potential years of life lost up to age 75 per 100,000 people among ages 0-74. Relative to a typical year, the U.S. lost an additional 3.6 million potential years of life in total in 2020.
The U.K. had the next closest premature excess death rate in 2020 with 488 excess potential years of life lost per 100,000 people, which is less than half the U.S. rate. Canada had the third highest premature excess death rate with 384 excess potential years of life lost per 100,000 people ages 0-74 in 2020, which is about one third of the U.S. rate.
The United States’ significantly higher excess death rate among younger age groups in 2020 causes it to have the highest premature excess death rate among peer nations. These premature excess deaths are in addition to the already high rate of potential years of life lost in the U.S. compared to peer nations in a typical year. The U.S. was among 5 peer countries (U.S., U.K., Canada, Austria, Belgium) with increased potential life years lost in the 15-64 age group in 2020, whereas the remaining peer countries actually saved life years in this age group in 2020 over a typical year. The COVID-19 pandemic led to higher excess death rate among people ages 15-74 in the U.S. than in peer countries. As noted above, while Belgium had the highest overall COVID-19 death rate and the second highest excess death rate among peer countries in 2020, the increased mortality rate in Belgium was largely due to a higher death rate among the elderly. Belgium ranked #5 among peer countries in premature excess death rate up to age 75, despite having the second-highest overall rate of excess mortality among peer countries because deaths in Belgium were more concentrated among older people.
The higher premature excess death rate in the U.S. was driven in part by racial disparities
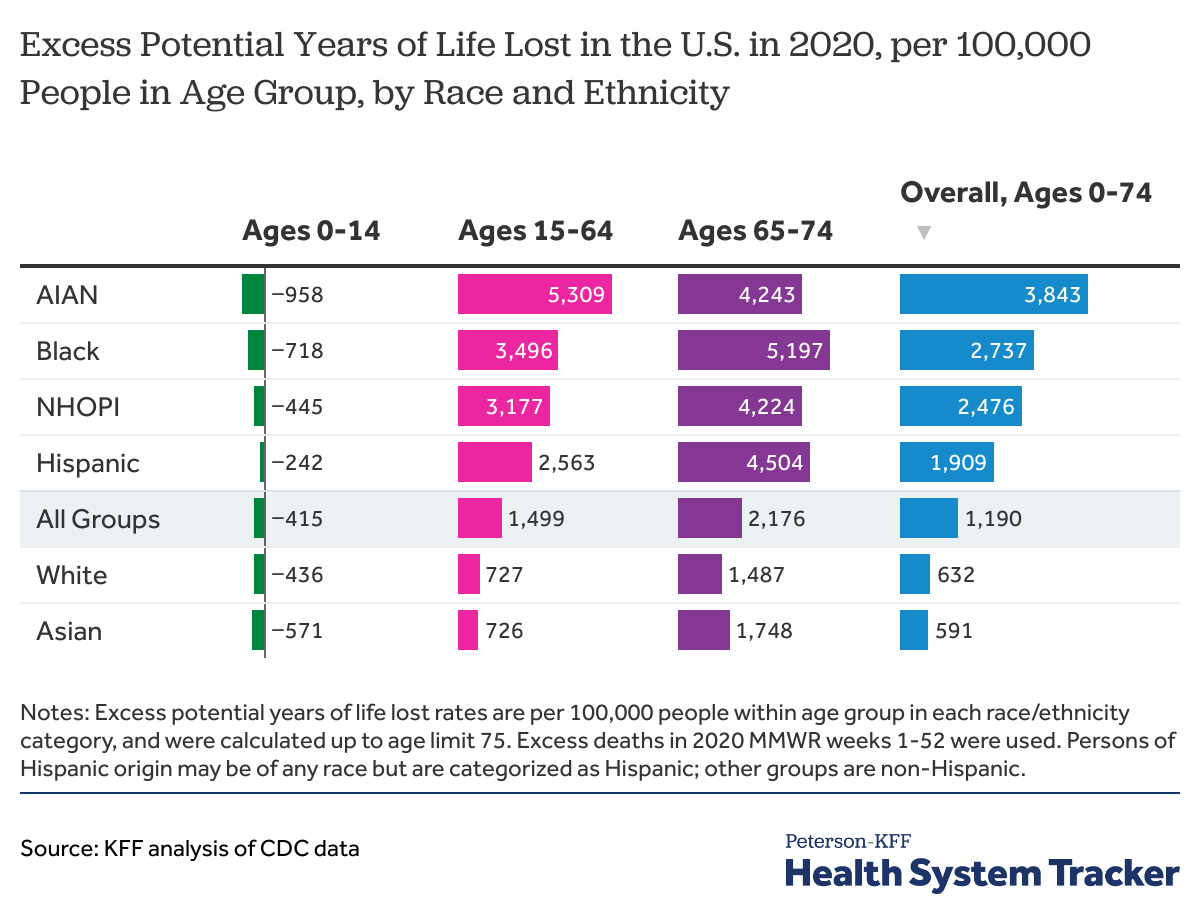
Using the CDC data on excess deaths by race and ethnicity and age groups, we find that American Indian and Alaska Native (AIAN), Black, Native Hawaiian and Other Pacific Islander (NHOPI), and Hispanic people had over 3 times premature excess deaths per 100,000 people in the U.S. in 2020 than the rate among White or Asian people. AIAN people ages 15-64 had the highest premature excess death rate (3,843), driving the 40% higher premature excess death rate among AIAN people ages 0-74 than the next highest group. The premature excess death rate was 2,737 among Black people ages 0-74, 2,737 among NHOPI people, and 2,476 among Hispanic people. Premature excess death rates among White and Asian people were lower than the overall rate, with 632 and 591 excess potential years lost per 100,000 people ages 0-74 in each group, respectively. Life expectancy already varied by race and ethnicity prior to the COVID-19 pandemic in the U.S. Life expectancy at birth in 2017 was 74.9 years, 78.5 years, and 81.8 years for Black, White, and Hispanic people, respectively. Of the 3.6 million excess potential years of life lost in the U.S. in 2020, 1.1 million excess life years were lost among Black people, another 1.1 million excess life years were lost among Hispanic people, and 1.1 million excess life years were lost among White people. As a share of the U.S. population, Black people represent 13%, Hispanic people represent 18%, and White people represent 60%.
Discussion
The pandemic appears to have significantly widened the gap in premature deaths in the U.S. and peer countries. Premature death rates in the U.S. were already higher than in peer countries prior to the pandemic. Our analysis of premature excess deaths indicates the gap in premature deaths between the U.S. and peer countries has increased due to the pandemic.
The higher excess mortality rate among younger people in the U.S. is likely due in part to higher COVID-19 risk factor rates among younger people in the U.S., and may also reflect differences in public health responses across countries. Over half of people hospitalized with COVID-19 in the U.S. had obesity, and the U.S. has by far the highest rate of obesity among peer countries. The majority of excess deaths in 2020 are directly attributable to COVID-19 and many of those excess deaths that are not attributed to COVID-19 may be undiagnosed COVID-19 deaths, particularly early in the pandemic when widespread testing was not available. However, higher rates of death from overdoses may also be a contributing factor to the United States’ high premature excess death rate in 2020, particularly among younger people.
The higher premature excess death rate in the U.S. compared to peer nations was driven in part due to racial disparities. Younger people of color were more likely to have died in the U.S. during the pandemic in 2020 than white non-elderly individuals. American Indian and Alaska Native, Black, Native Hawaiian and Other Pacific Islander, and Hispanic people had over 3 times the premature excess death rate in the U.S. in 2020 than the rate among other groups. American Indian and Alaska Native people had a 40% higher premature excess death rate over the next highest group.
Additional analysis of CDC data shows that COVID-19 was the third leading cause of death among people ages 65 and over, and the fourth leading cause among people younger than 65 years in 2020. During the winter surge, in December 2020 and January 2021, COVID-19 was the leading cause of death both among people younger than 65 and those ages 65 and over in the U.S.
The COVID-19 pandemic has affected the health of populations and economies in the U.S. and elsewhere. To be sure, the elderly are at the highest risk of death from COVID-19 infection. However, the COVID-19 pandemic has not left younger people unharmed. Among peer nations, the U.S. had the highest excess mortality rate of non-elderly adults in 2020, and therefore, had the highest increase in premature death rate among peer countries in 2020. Although prevention measures have been weighed against the impact on the economy, loss of non-elderly adults may also have an impact on long-term economic productivity. Even after many of the elderly at the highest risk of serious illness from COVID-19 infection are vaccinated, social distancing measures will continue to be important to prevent infection, serious illness, hospitalizations, and deaths among unvaccinated younger people, as well as to mitigate long-term economic impacts for non-elderly adults.
Methods
The Human Mortality Database Short-term Mortality Fluctuations (STMF) data were used to calculate the excess deaths through the 2020 MMWR week 52 in peer countries by age groups. Excess deaths were calculated as the deaths in 2020 over the average deaths in 2016-2019. Age-specific data for Australia and Canada were only available through 2020 weeks 47 and 51, respectively. Excess death data for Japan were not available in the Human Mortality Database. For the country comparison, excess potential years of life lost were calculated by summing the number of excess deaths within each age group. Then, those counts were multiplied by the number of years from the mid-point of the age range up to 75 years. Although average life expectancy among peer countries is higher, from 78.7 years in the U.S. up to 84.2 years in Japan, we used 75 years based on the OECD methodology. Potential remaining years were calculated from 8, 50, and 69.5 years to the age limit for age groups 0-14, 15-64, and 65-74, respectively. U.S. CDC data show that weighted average excess death age in the 15-64 age group is 50 years. Because more granular age data for excess deaths were not available in all countries, we used an age of 50 to calculate potential years of life lost to the age limit of 75 for the 15-64 age group for all countries. This decision might make the gap between the U.S. and peer countries smaller as the age at excess death in peer countries might be higher than 50 years. Lastly, excess years of life lost were combined across all age groups for the excess potential years of life lost in each nation. For each country, excess potential years of life lost were calculated per 100,000 people in each country using the 2018 OECD population counts by age groups.
CDC excess death data by age groups and week were used to assess excess deaths within age groups and portion of excess deaths attributed to COVID-19 in the U.S. CDC data were also used for analysis of excess deaths and excess potential years of life lost by race and ethnicity groups in the U.S. in 2020. Excess deaths in 2020 MMWR weeks 1-52 were used for calculation of excess mortality rate by race and ethnicity. For excess potential years of life lost calculation, excess death counts were multiplied by the distance between the mid-point of the age groups to the age limit and summed within each age and race or ethnicity group. Persons of Hispanic origin may be of any race but are categorized as Hispanic; other groups are non-Hispanic. CDC data on population counts by age and race or ethnicity were used to standardize premature excess deaths per 100,000 people.
A limitation of this analysis is that the excess potential years of life lost were based on excess deaths by age groups rather than excess deaths at each age. Our results of excess potential years of life lost are similar to other earlier studies of potential years of life lost in the U.S. due to COVID-19. Our estimates of excess potential years of life lost are likely underestimated due to a few reasons. First, although we limited the excess years lost calculation up to age limit of 75, excess deaths above 75 years are also premature deaths by some amount of time; therefore, estimates presented here are likely underestimated for the overall excess potential years of life lost. Second, we incorporated excess life years saved among the youngest ages 0-14 in the overall estimate. Deaths among children ages 0-14 decreased in 2020 in most countries compared to prior years. Early reports indicate deaths due to accidents and influenza have been lower among children due to social distancing and lockdown measures implemented during the pandemic.
The Peterson Center on Healthcare and KFF are partnering to monitor how well the U.S. healthcare system is performing in terms of quality and cost.