NOTE: This analysis was updated in March 2022.
The initial roll out of COVID-19 vaccines in the United States has been mired with distribution challenges. State and local governments, health systems, and other providers have at many times faced shortages and other times been left with unused vaccines. One of the vaccines authorized thus far, the Pfizer-BioNTech vaccine, has specific storage requirements, which also creates challenges for some locations. Priority groups eligible to get vaccinated have found the process difficult to navigate. Communication between federal and local officials might have improved recently, but vaccine supply bottlenecks remain and racial disparities in access have emerged. Understanding where adults got vaccinated before the pandemic can inform the massive state and federal efforts to vaccinate Americans against COVID-19. Accessibility of vaccination locations is one component that will influence equity in COVID-19 vaccination rates.
Where vaccinations are provided may also affect payers’ costs for COVID-19 vaccine administration. The federal government centrally pre-paid for COVID-19 vaccine doses but some of the costs of administering the vaccines will fall on payers. Whether vaccine recipients are insured through a private insurer or a public program, or are uninsured, they will face no out-of-pocket costs for the vaccine or its administration. For the near future, providers will receive COVID-19 vaccines from the federal government at no cost. Providers will, however, often bill public and private payers for the cost of administering the vaccines (i.e., the cost of paying staff to give the shot). Insurers are then required to pay for the charges of administering the vaccine without imposing cost-sharing. For out-of-network providers, CMS has suggested payers use a reasonable payment rate, or the Medicare payment amount. Providers are able to use the COVID Provider Relief Funds to cover vaccine administration costs for uninsured patients, as well as any excess costs not fully reimbursed by payers. The cost of COVID-19 vaccine administration will likely have an upward effect on claims costs in 2021, as several insurers noted in their rate filings to state regulators.
In early April 2022, the U.S. federal government will run out of funds to pay for COVID-19 vaccines and vaccine administration costs for uninsured and underinsured people.
This brief shows where Americans typically get flu vaccines in the U.S. and how much it costs to administer flu and other vaccines using data from past years. We use 2018 Behavioral Risk Factor Surveillance System (BRFSS) data on where adults typically get flu shots, and 2018 MarketScan data for administration costs of flu and other vaccines among non-elderly adults with employer coverage. Where and how many adults get the COVID-19 vaccine is going to be different than for flu because COVID-19 is more serious and COVID-19 vaccine doses are more limited. We focus on flu vaccine location because flu vaccines are recommended to almost everyone and given to a large share of the population each year. Understanding how Americans access flu vaccines can inform policymakers about which sites may be effective for reaching people for COVID-19 vaccinations, particularly as distribution points increase. We focus on adults because children have specific vaccine regimens and differ from adults as to where they get vaccines. Additionally, COVID-19 vaccines are thus far only authorized for ages over 16 (Pfizer-BioNTech vaccine) and over 18 (Moderna COVID-19 vaccine).
Most people get flu vaccines at a doctor’s office or retail health clinic
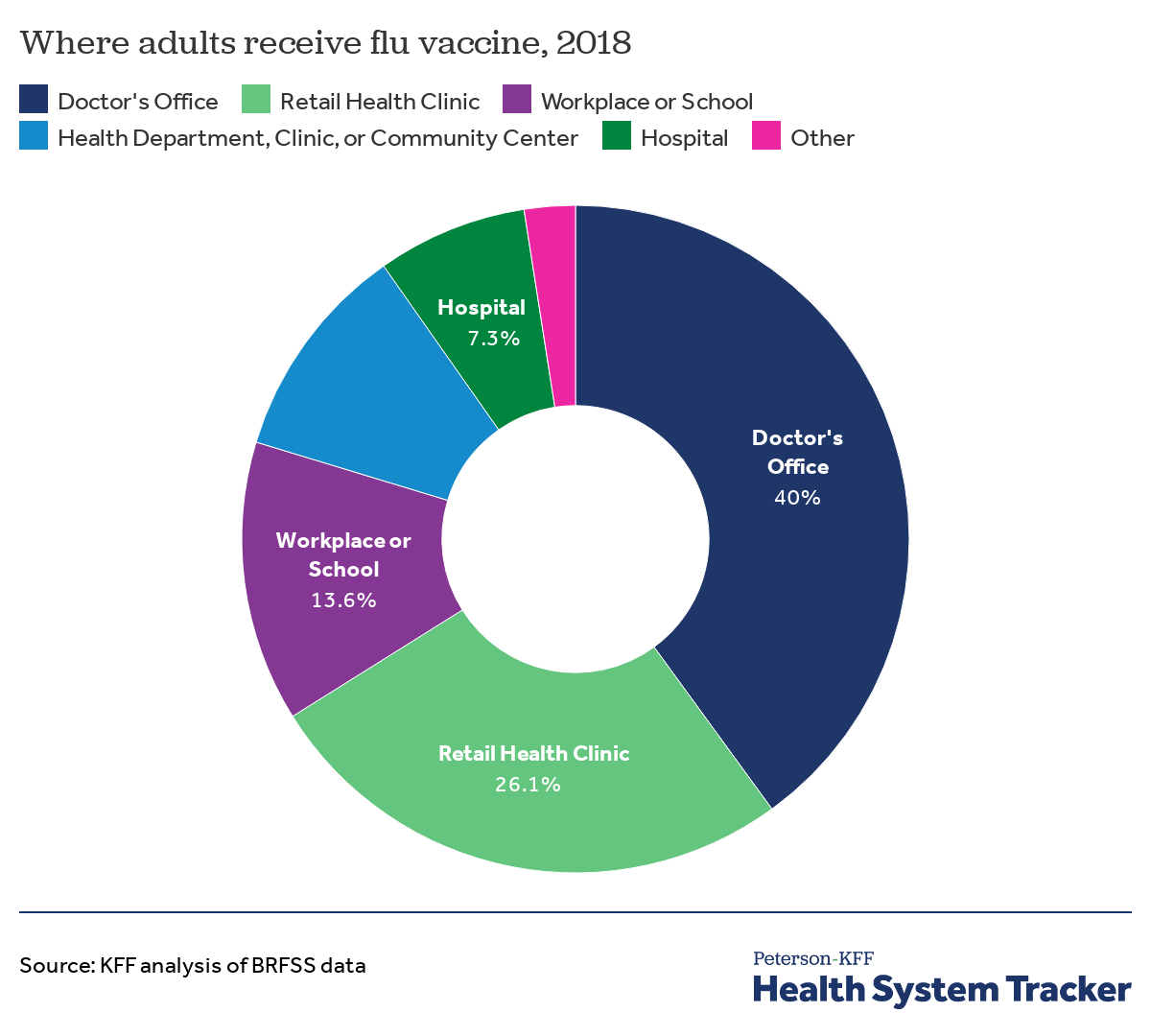
About half of American adults reported getting a flu shot during the 2019-2020 flu season with differences in uptake across a variety of demographic groups. In 2018 survey data (BRFSS does not collect flu shot location data for each year), most adults reported getting a flu shot at a doctor’s office (40%) or a retail pharmacy or store health clinic (26.1%). The remaining adults who reported getting a flu shot received it through their workplace or school (13.6%), through a public health department clinic or community health center (10.6%), or at a hospital (7.3%).
Because some in-person workplaces and schools have been closed due to social distancing recommendations, federal and local officials will need to consider how to get COVID-19 vaccines to those who would have generally gotten vaccinated at workplaces or schools. Schools and other community sites can be used as mass vaccination sites as well.
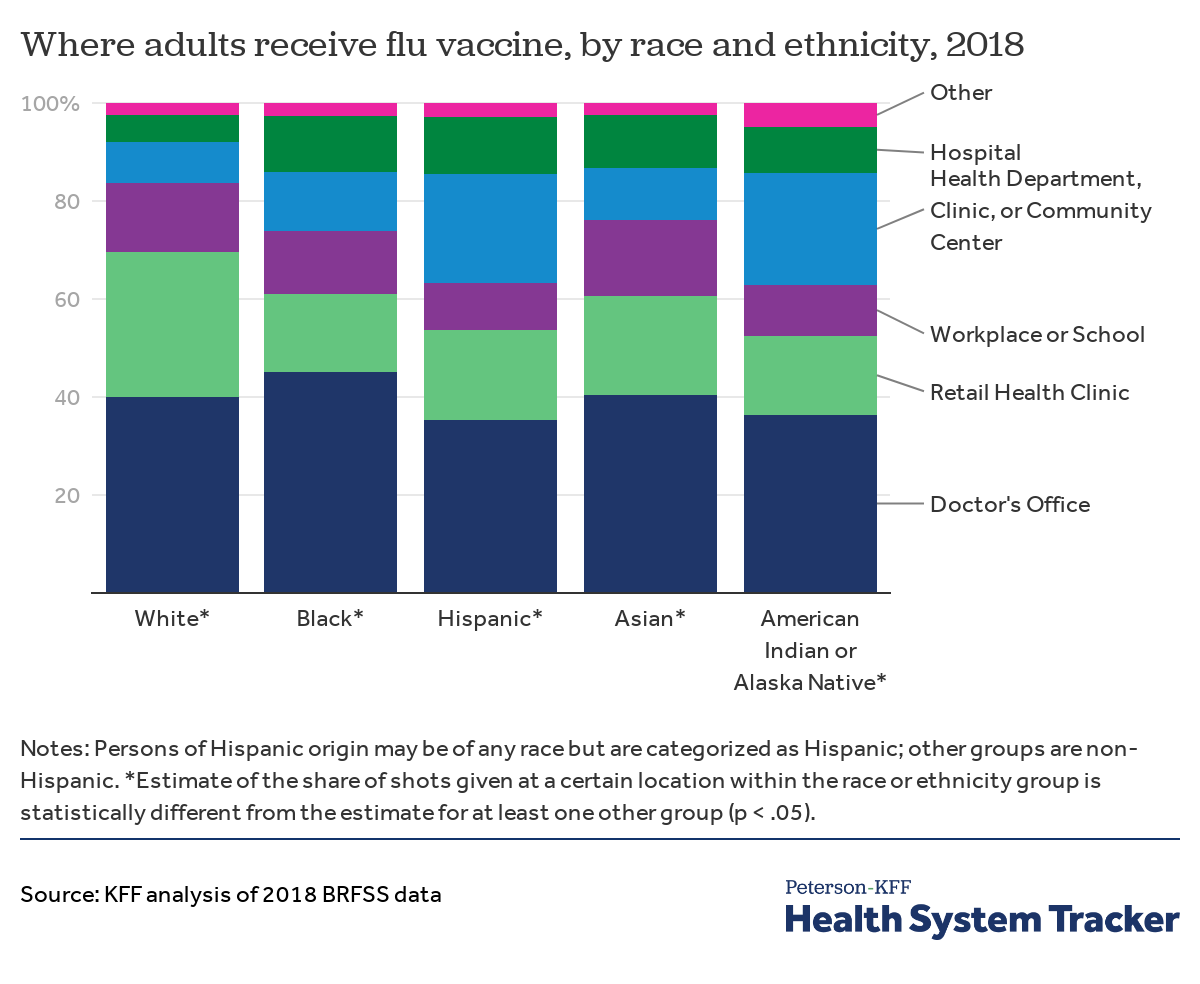
Where Americans typically get the flu vaccine varies by race and ethnicity
Across racial and ethnic groups, most adults reported receiving a flu vaccine at a doctor’s office. Retail health clinics were also a primary vaccination site for White adults, with 30% receiving their flu vaccine through a retail pharmacy or store. In contrast, Black, Hispanic, Asian, and American Indian or Alaska Native adults were all less likely than White adults to receive a flu vaccine at a retail health clinic. Compared to White adults, a higher share of Hispanic and American Indian or Alaska Native adults reported getting a flu vaccine at a public health department, clinic, or community health center.
KFF analysis has raised early concerns about racial disparities in COVID-19 vaccinations. The findings in this analysis suggest that as the COVID-19 vaccine becomes more widely available, decisions about where people can access the vaccine will have implications for racial equity. Specifically, the data suggest that distribution through retail pharmacies may disadvantage people of color since they have been less likely to use retail clinics as a location to get flu shots. In contrast, making the vaccine available through doctors’ offices and health departments, clinics, and community health centers may facilitate access for people of color given that these have been the primary sites through which they receive their flu vaccination. Moreover, other KFF research shows that health care providers are a top source that people say they will turn to for help with vaccine decision-making across racial and ethnic groups.
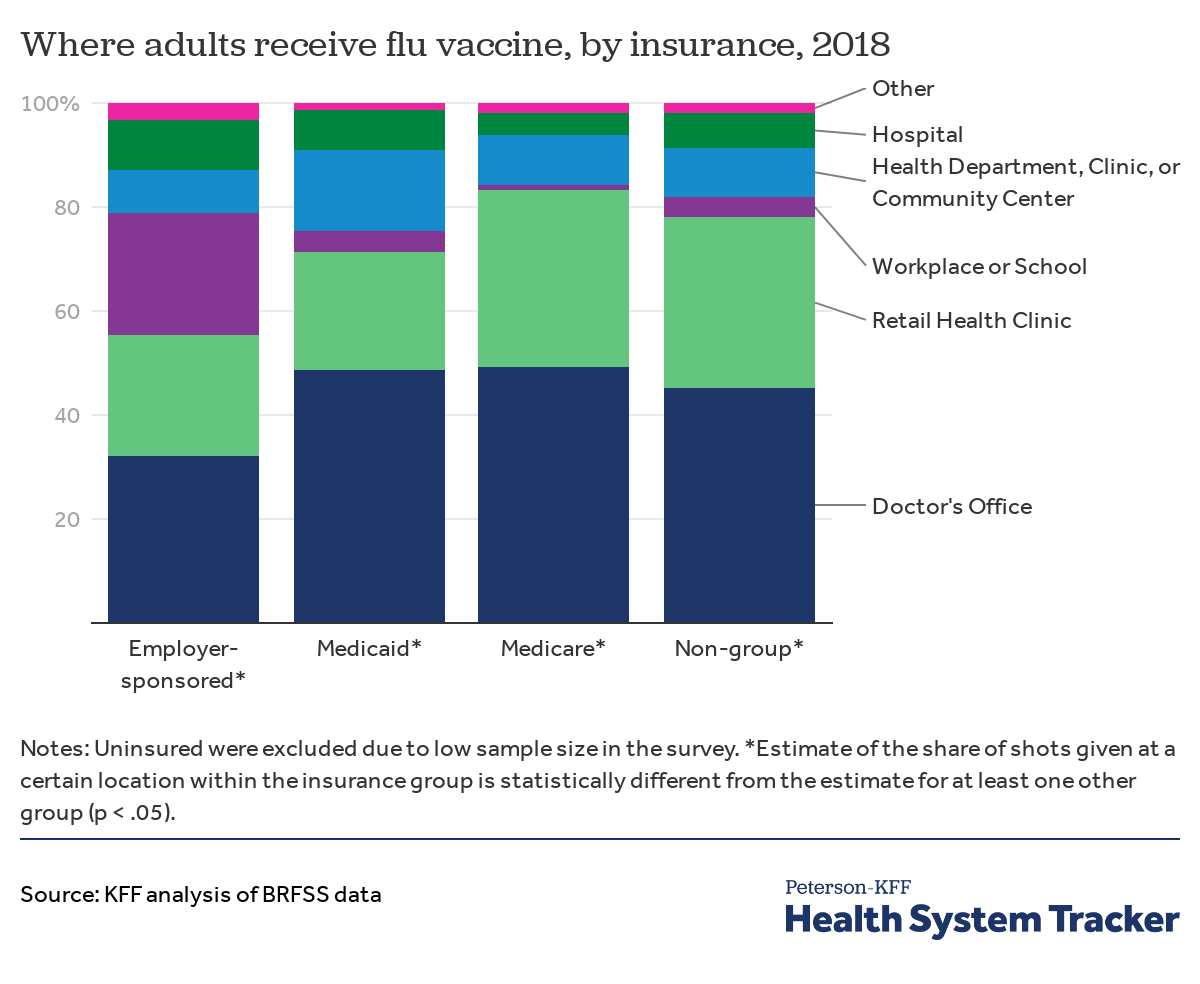
Among those insured through an employer plan, almost a fourth received the flu vaccine at work
While most adults received the flu shot through a doctor’s office or a retail clinic, almost one in four (24%) adults insured through their employers reported receiving the flu vaccine at their workplace or school. Less than 5% of adults insured through Medicaid, Medicare, or non-group insurance reported getting flu shots through their workplaces or schools. A higher share of individuals covered by Medicare and Medicaid went to a doctor’s office to receive their vaccination.
Particularly early on in the rollout of COVID-19 vaccines, Americans will end up getting the COVID-19 vaccine where they are able to, based more on how localities funnel vaccination doses than on their source of insurance. However, in the long run, when vaccinations become more widely available, insurance type, which is correlated with the usual source of care, may play a bigger role in where Americans go to get the COVID-19 vaccine.
The typical payment for administering a vaccine is about $25, and vaccines requiring two doses could cost $50 to administer in total
The federal government has stated the COVID-19 vaccines will be available to Americans at zero cost, regardless of their insurance status. Where people end up receiving the vaccine (e.g., at a doctor’s office vs. a mass vaccination site) may affect whether their insurance is billed for the cost of administering the dose.
With millions of doses being administered, administration costs will add up. Some COVID vaccines include a two-dose schedule. While the cost of administering other vaccines might not be perfectly analogous, it could give a general idea of how much administering each individual dose might cost.
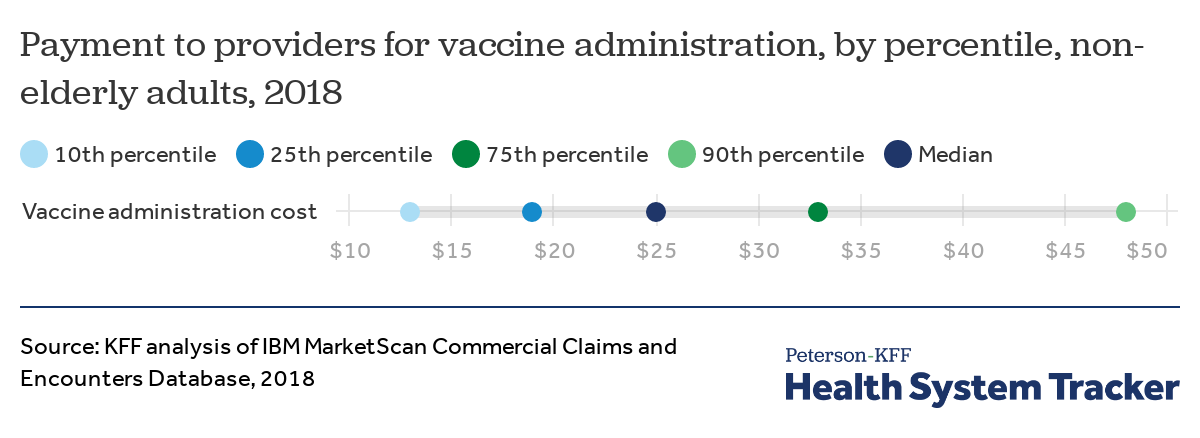
This chart shows the cost of administering all adult vaccines. We did not limit this chart to only flu shots because insurers’ payments to providers for administering a shot are similar regardless of the vaccine.
Among non-elderly adults with private health insurance through a large employer, plan payments for administering a vaccine at a doctor’s office ranged from $13 at the 10th percentile to $48 at the 90th percentile with a median payment of $25 in 2018. This suggests that COVID vaccines with two doses will likely cost private insurers around $50 to administer per person in sum.
Medicare was previously paying providers $28.39 for administering a COVID-19 vaccine requiring a single dose, which is similar to the $25 private insurers typically pay per vaccine administered. Since the end of 2021, Medicare has been paying providers $40 per vaccine shot administered for most patients. Additionally, CMS has said the Provider Relief Fund can be used to cover COVID vaccine administration costs in excess of payer reimbursements and for uninsured patients.
After the U.S. federal government runs out of funds that covered the cost of vaccine administration on April 5, 2022, uninsured and underinsured people may be charged for COVID-19 vaccine administration at a rate similar to those charged for Medicare. Vaccine administration costs are required to be covered by the insurer or payer for other publicly or privately insured people.
Conclusion
Where people are able to access the COVID-19 vaccine will have important implications for access and equity. Among Americans who got a flu vaccine, most adults got it at a doctor’s office or retail clinic (pharmacy or store). However, a greater share of Hispanic and American Indian or Alaska Native adults reported getting a flu shot at a local health department, clinic, or community health center than the share of White adults. Additionally, a lower share of Black, Hispanic, Asian, and American Indian or Alaska Native adults reported getting a flu shot at a retail clinic than the share of White adults.
COVID-19 vaccine rollout began with vaccines initially being provided at hospitals and long-term care facilities. As states and localities continue to roll out the COVID-19 vaccine to broader groups of the population, additional sites and locations have been designated. The Biden Administration’s COVID-19 relief plan includes increasing the number of vaccine administrators and vaccination sites. Building on partnerships initiated during the Trump Administration, the Biden Administration is activating pharmacy partnerships to allow those eligible to get vaccinated at local pharmacies starting on February 11. The Biden Administration has also recently announced partnering with community health centers. Some cities have begun using mass vaccination sites (e.g., athletic stadiums) to administer the vaccine. The reach and equity of COVID-19 vaccination efforts could be improved by providing COVID vaccines at community locations that people trust, such as, community health departments or clinics, community recreation centers, places of worship, and local schools.
While the federal government will distribute COVID-19 vaccines to states and providers at no cost, providers may bill public and private insurers for the cost of administering the vaccines. Our analysis of large employer plans’ payments for flu and other vaccines shows that the typical cost of administering vaccines in private plans is similar to the rate Medicare plans to pay providers for administering the COVID-19 vaccine. Although there is still some uncertainty about how the cost of administering the vaccine will be spread across state and local governments and private insurers, individuals will receive COVID vaccines at no cost to them. In many cases, health plans will have to pay providers for the cost of administering each vaccine, which, depending on the vaccination rate and timing, could have an effect on premiums next year. However, premiums for this year have generally been set by private insurers and employers.
Methods
The 2018 CDC Behavioral Risk Factor Surveillance System (BRFSS) data were used to assess how many adults received the vaccine (FLUSHOT6) and where they received the flu vaccine (IMFVPLAC) in the prior 12-months. BRFSS is an ongoing, state-based, random-digit-dialed telephone survey of non-institutionalized civilian adults aged 18 years and older. Guam and Puerto Rico were excluded. Place of flu vaccine for adults is collected in BRFSS every 3rd year, and therefore, the most recent survey year with data on flu vaccine location, 2018, was used for this analysis. In the analysis by race or ethnicity, persons of Hispanic origin may be of any race but are categorized as Hispanic; all other groups are non-Hispanic. One limitation of using self-reported data is there may be differences in how people describe getting the flu shot. For example, it is possible survey respondents referred to a health department, clinic, or community center as a doctor’s office – or vice versa.
The 2018 IBM MarketScan Commercial Claims and Encounters Database was used to assess the total payments for vaccine administration for non-elderly adults in the office-based setting. MarketScan contains claims data for those enrolled in large employer-sponsored plans. Those receiving vaccines other than in office-based settings were excluded. We estimated the cost of vaccine administration (procedure codes: 90460, 90461, 90471 through 90474, G0008, G0009, G0010) on days with a claim for one of several vaccines (including influenza (flu), hepatitis A and B, and others). Claims with adjusted or cancelled claims on the same day were excluded.
The Peterson Center on Healthcare and KFF are partnering to monitor how well the U.S. healthcare system is performing in terms of quality and cost.