It is well documented that the U.S. is an outlier among peer countries when it comes to health spending, and recent Peterson-KFF analysis finds that the cost of inpatient and outpatient care is the primary driver behind this gap in health expenditures. In addition, countless news articles have highlighted extremely high medical bills sent to patients, often resulting from balance billing from out-of-network providers. However, the actual costs of specific healthcare services in the U.S. are often hard to track down and can vary widely between plans and across the country.
In this analysis, we explore the average cost of several common healthcare services in the U.S. We analyzed data from a sample of the IBM MarketScan Commercial Claims and Encounters Database, which includes health claims from non-elderly people enrolled in large employer plans. When possible, we show how these costs have changed over time and how they vary geographically.
The charts in this analysis show average allowed amounts large employer health plans agree to pay for in-network and out-of-network care. We refer to “cost” as the weighted average total expenditures made towards a given admission or service, including the portion paid by the health plan and any out-of-pocket costs paid by enrollees under the plan’s cost sharing. However, the charts do not include any balance bills (“surprise bills”) that out-of-network providers may send directly to patients.
This collection demonstrates that the costs associated with many common health services have risen more rapidly than general economic inflation, and that there are large geographic variations in the cost of the same health services across the United States. For example:
- The average cost of a hospital admission among large employer plans increased by roughly $10,000 (68%) from 2008 to 2018
- Over the same period, the average cost for a laparoscopic appendectomy increased nearly five times faster than inflation
- The average cost for a lower back MRI is nearly three times higher in the Houston, TX area ($1,106) than in the Las Vegas, NV area ($404)
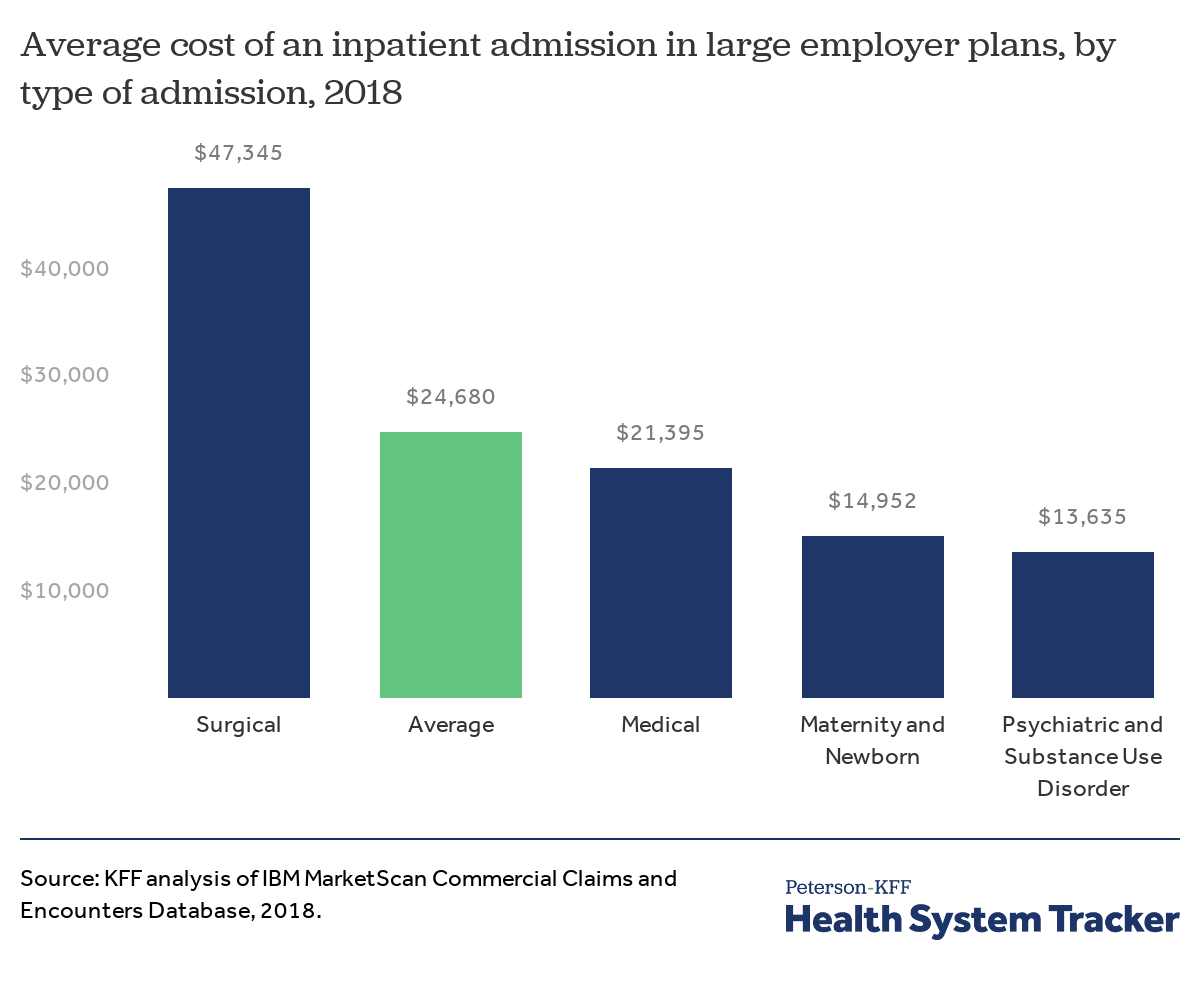
There is wide variation in the cost of inpatient hospital admissions depending on the type of Admission
The average cost of an inpatient hospital admission for people with large employer coverage was $24,680 in 2018. The cost of a hospitalization varies widely, depending on the reason for the admission. Maternity and newborn admissions, for example, average $14,952, while the cost of a surgical admission is much higher, averaging $47,345. For the purposes of this analysis, the cost of an inpatient admission includes the cost of professional services provided by physicians or hospital staff as well as any drugs that may have been administered during the hospital stay.
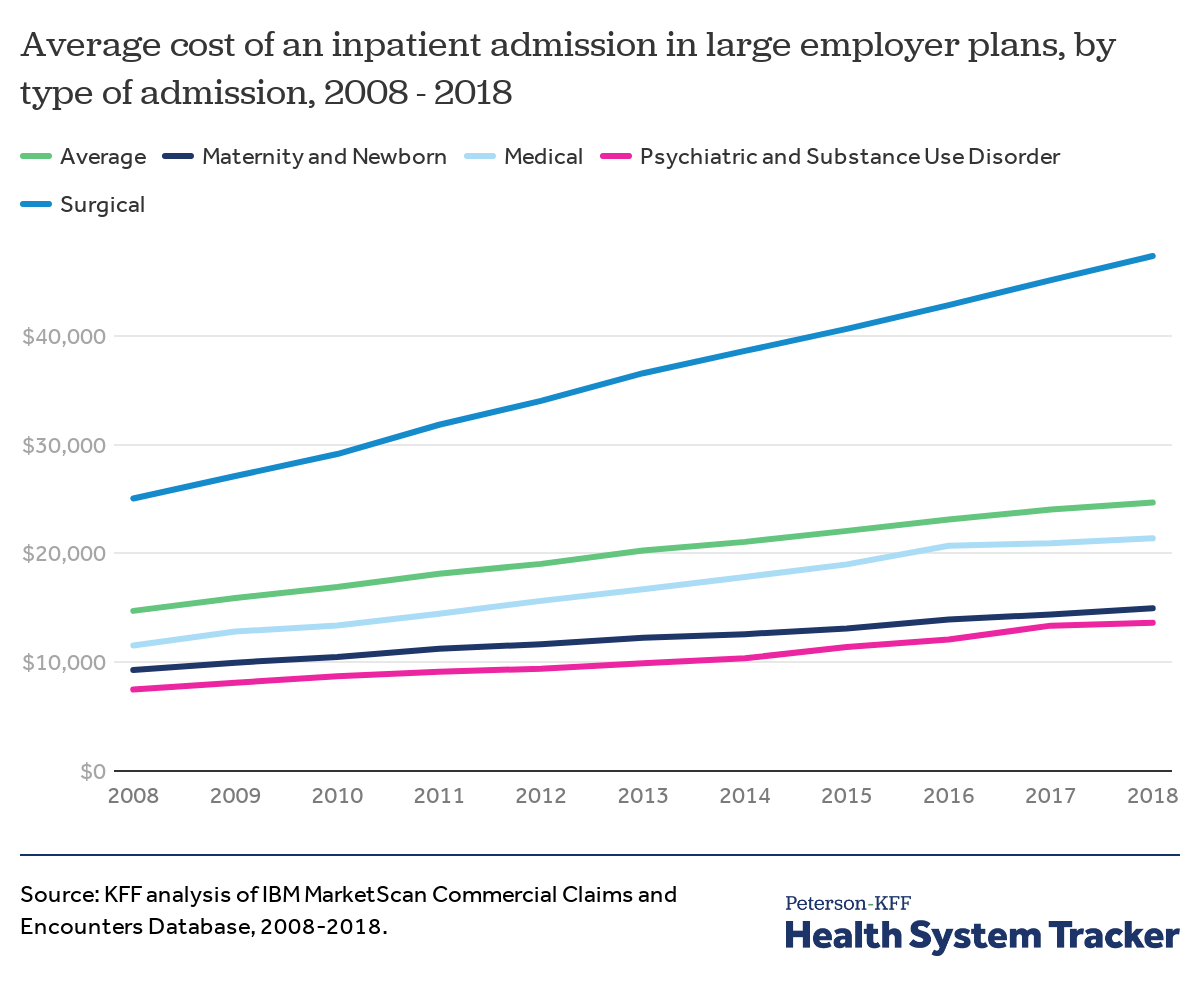
The cost of inpatient hospital admissions for surgical and medical care nearly doubled from 2008 to 2018
Among people with large employer coverage, the average cost of inpatient hospital admissions has increased by nearly $10,000 (68%) since 2008. Inpatient admissions for surgical care experienced the steepest cost increases, rising by $22,291 (89%) over the decade. General medical admission costs also rose steeply, by $9,850, or 85%, over the decade. Psychiatric and substance use admissions also increased in cost by $6,139 (82%). For reference, inflation increased 17% over the same period.
The cost of an inpatient admission varied by location in 2008 and 2018
The cost of an inpatient admission has increased across all regions since 2008. The chart above shows the average cost of an inpatient admission across the 25 Metropolitan Statistical Areas (MSAs) with the highest number of inpatient admissions among large employer plans in 2018.
On average, inpatient hospital admissions were most expensive in the San Diego, CA, area in both 2008 and 2018. The least expensive areas for an inpatient stay also remained constant over that period – St. Louis, MO and the Louisville area in KY and IN.
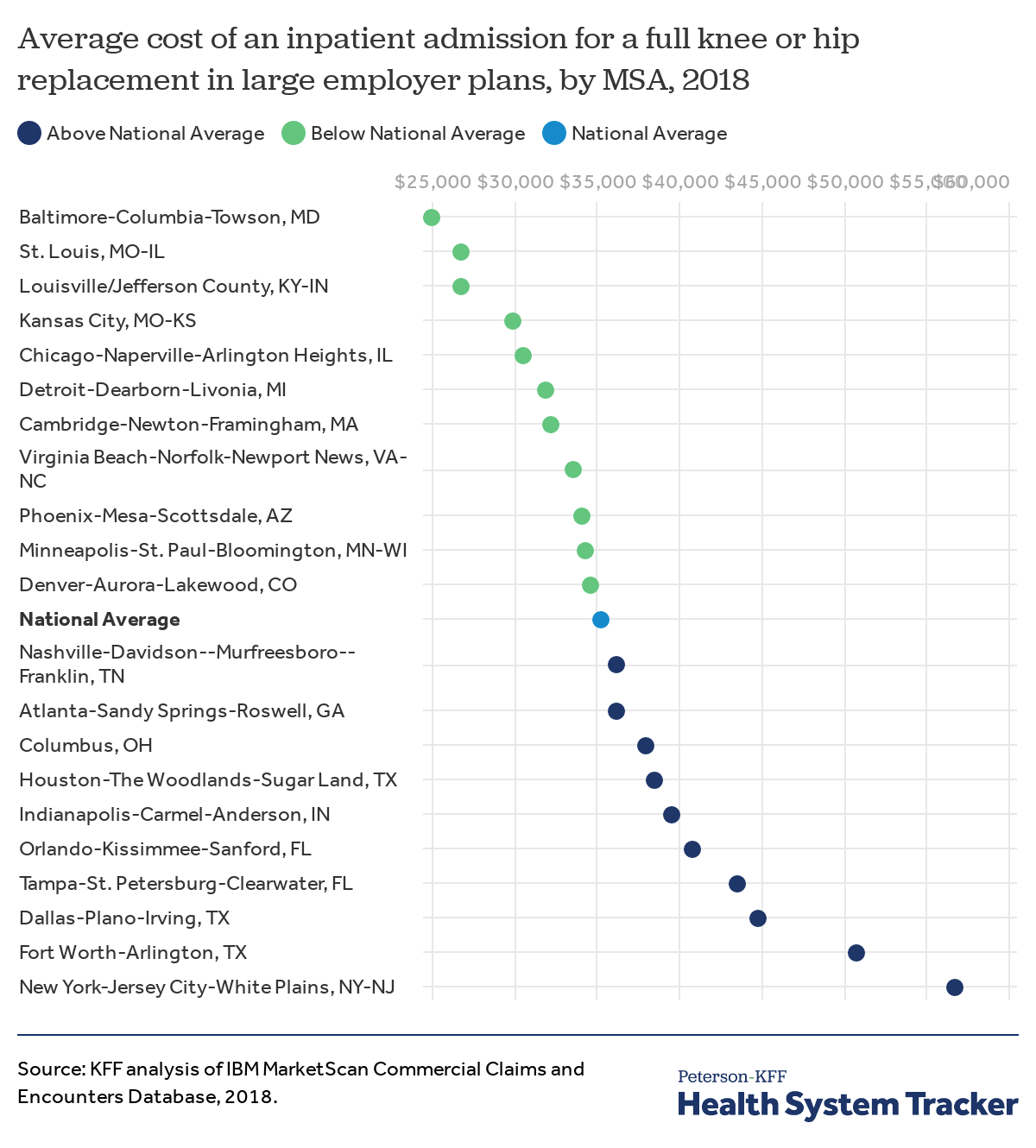
The average cost of full knee or hip replacements varies considerably across markets
This figure shows the average cost of an inpatient admission for a full knee or hip replacement in most populous MSAs with more than 125 procedures in 2018. There is considerable geographic variation in the average cost paid by large employer plans and their enrollees for these surgeries. For instance, the average cost of a full knee or hip replacement in the New York City area is $56,739, which is 127% higher than the average cost in the Baltimore area ($25,044) and 61% higher than the national average ($35,263).
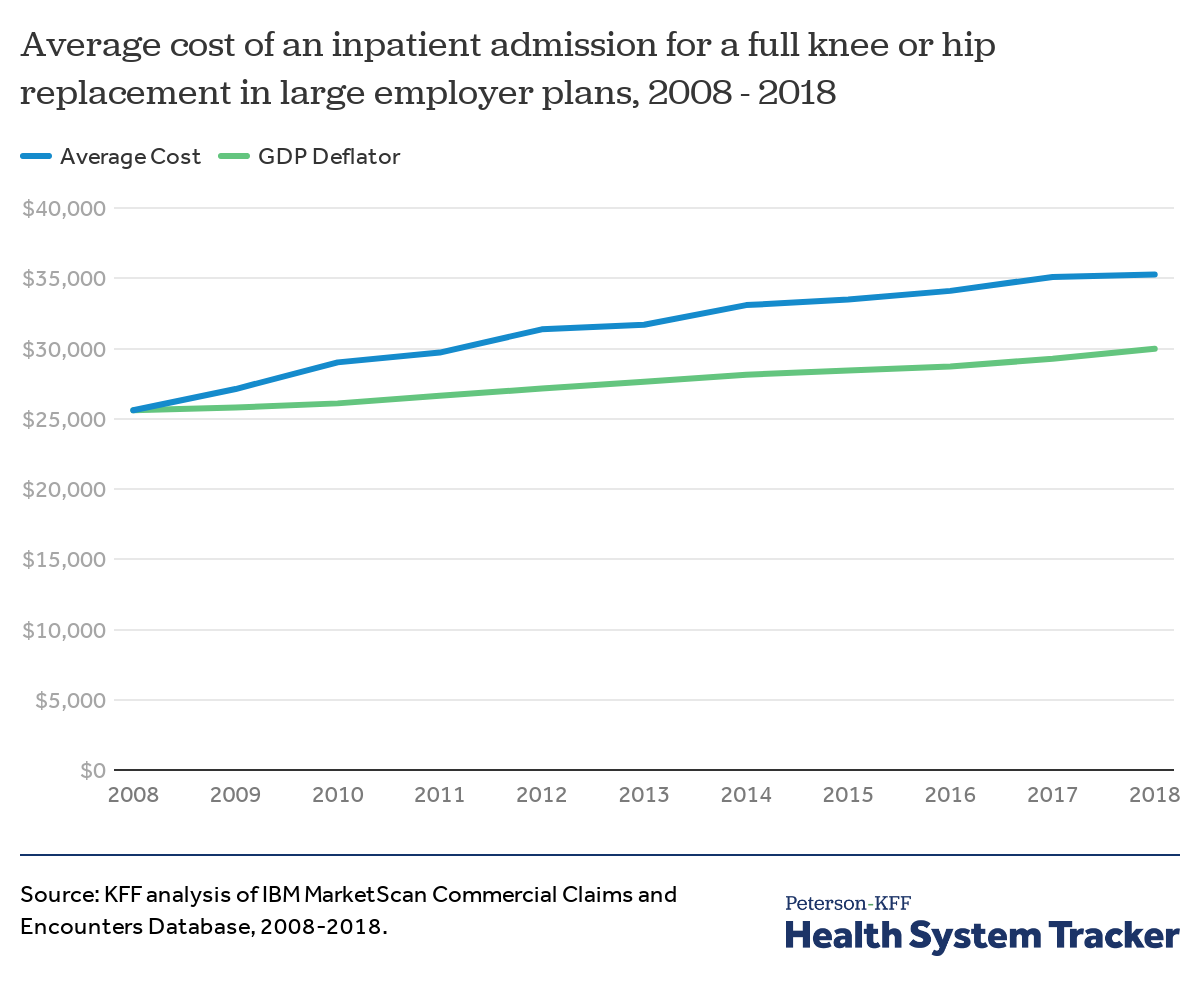
The average cost of a full knee or hip replacement has increased faster than other prices in the economy
The average cost of an inpatient admission for a full knee or hip replacement increased 38% (or $9,662) from 2008 to 2018, compared to a 17% increase in inflation over the same period (as measured by the GDP deflator).
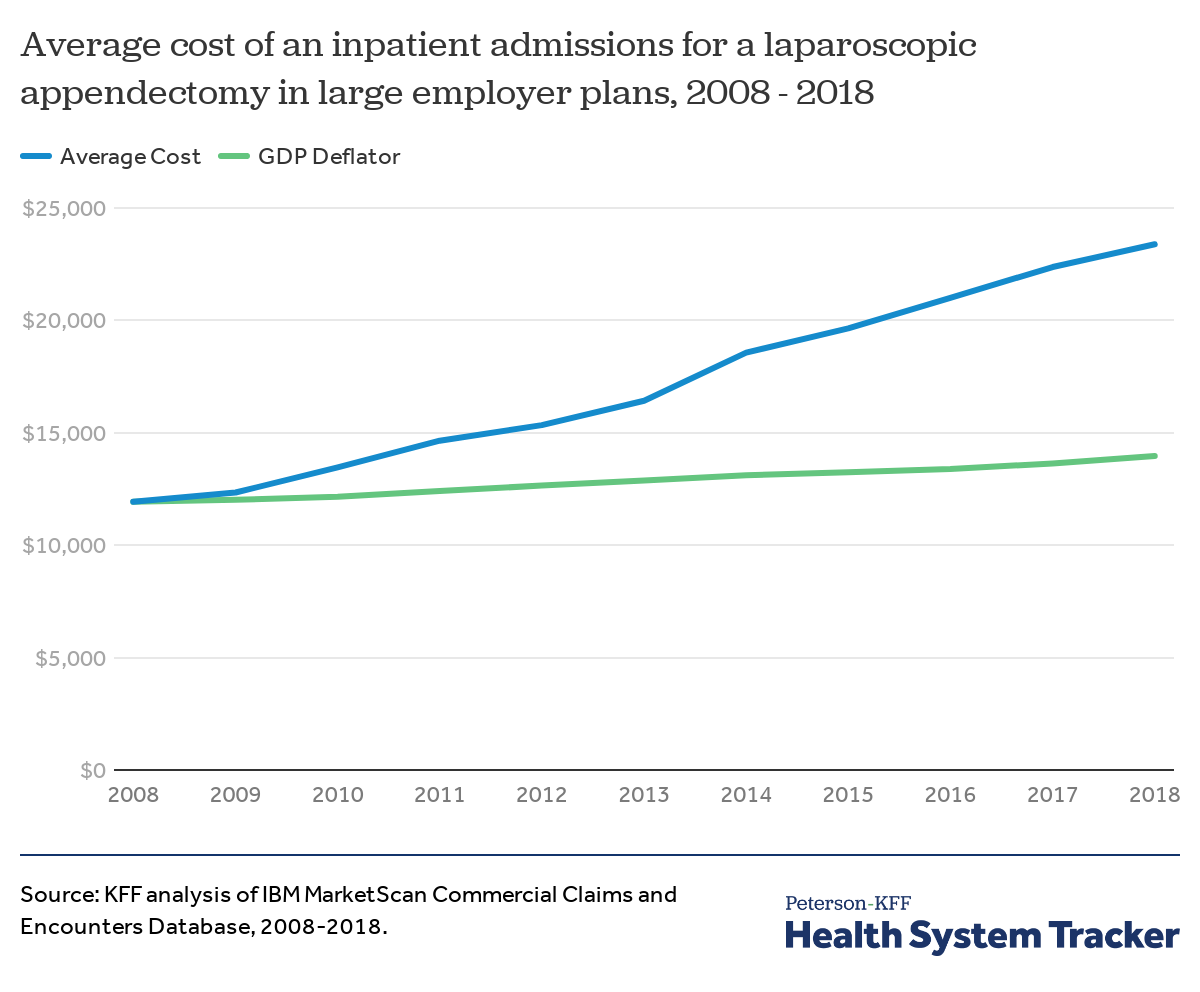
The average cost of a laparoscopic appendectomy procedure has increased far faster than general inflation
Among large employer plans, the average cost of an inpatient admission for a laparoscopic appendectomy was $23,385 in 2018. The average cost for a laparoscopic appendectomy nearly doubled from 2008 to 2018 (increase of $11,456 or 96%), growing much faster than inflation over the same period (17%).
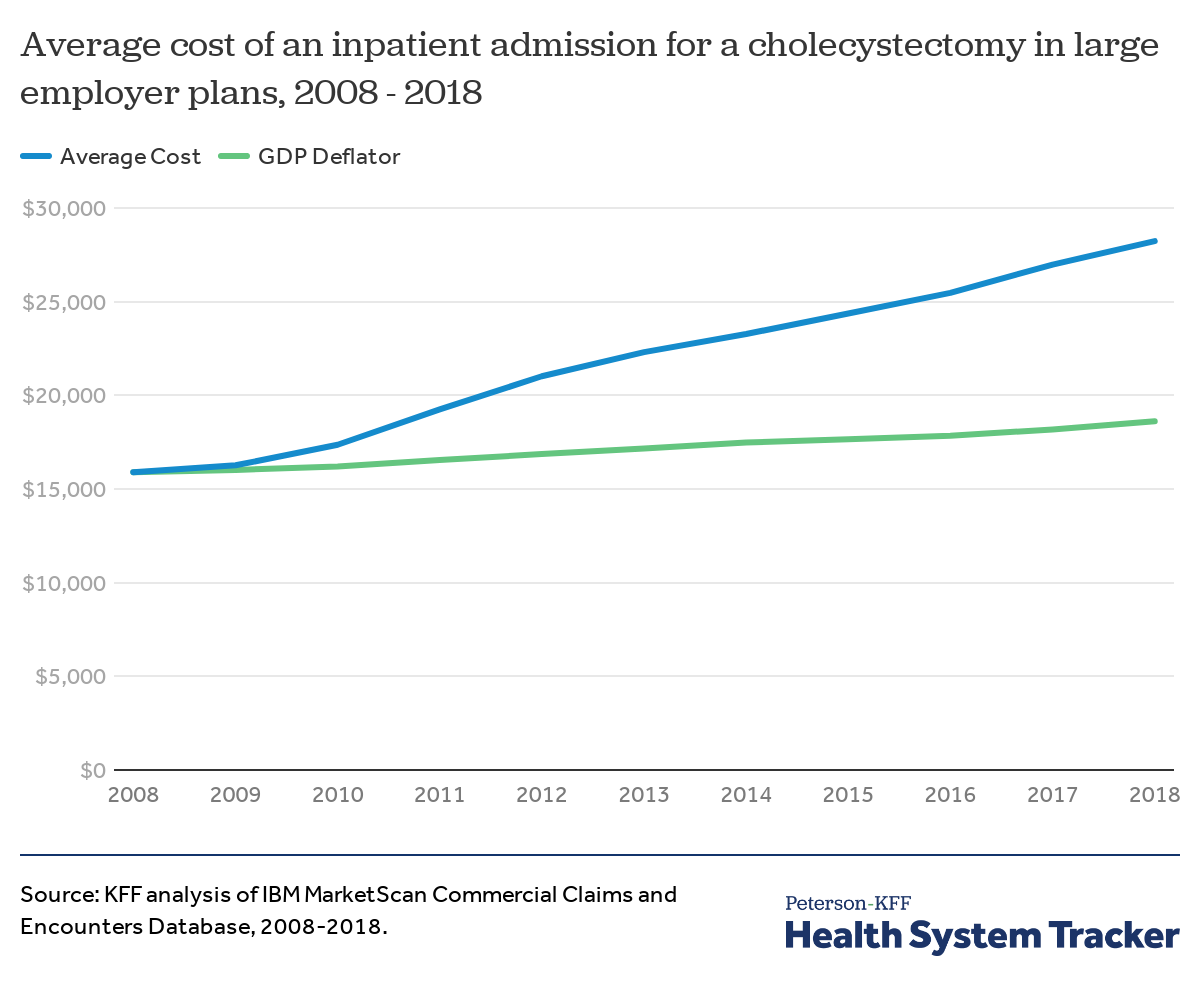
The average cost of laparoscopic gallbladder removal surgery has increased more than four times faster than general inflation.
A laparoscopic cholecystectomy involves the surgical removal of the gallbladder. The cost of an inpatient admission for this surgery nearly doubled from $15,900 in 2008 to $28,233 in 2018 – an increase of 78% over ten years, which was more than four times faster than inflation (17%).
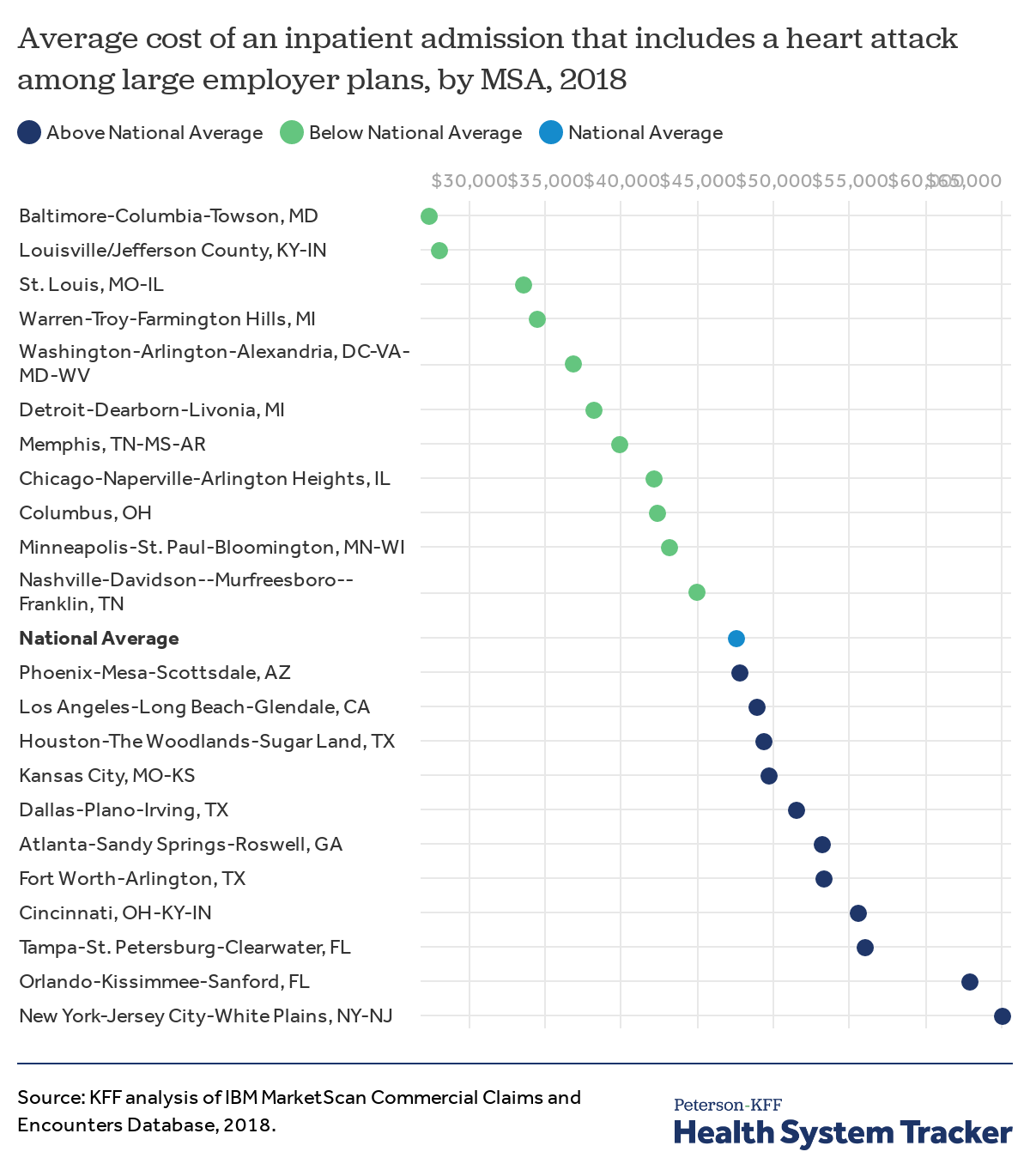
The average cost of an inpatient admission that includes a heart attack costs more than twice as much in the New York City area than in the Baltimore area
There is considerable geographic variation in the average cost paid among large employer plans for an inpatient hospitalization that includes a heart attack. For instance, the average cost of a hospital stay that includes a heart attack in the New York area is $65,138, which is 37% higher than the national average ($47,666) and 137% higher than the average cost in the Baltimore area ($27,434).
The Baltimore area has lower-than-average costs for many inpatient admissions, including the lowest average cost for knee or hip replacements and inpatient admissions related to a heart attack. These lower inpatient prices may be due in part to Maryland’s all payer rate setting program.
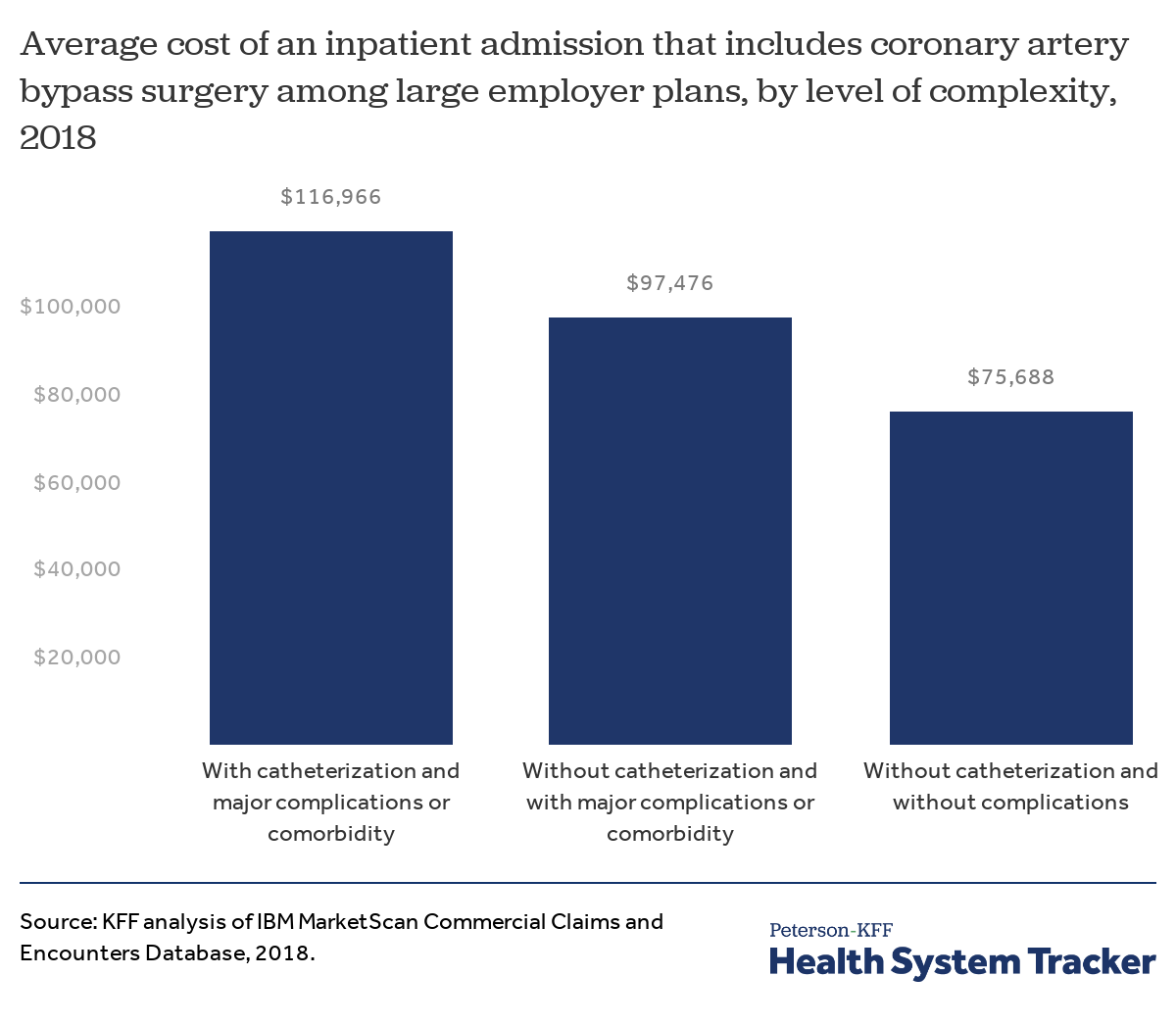
Inpatient admissions for cardiac problems that require invasive surgical procedures can be much more expensive
Coronary artery disease— the buildup of plaque leading to reduced blood flow to the heart— forms the pathogenic basis for heart disease and heart attacks, the leading cause of death in the United States and a major driver of health spending.
Common treatments for these conditions aim to circumvent blockages in the arteries, and include cardiac catheterization and coronary artery bypass graft surgery (bypass surgery). Cardiac catheterization involves injecting a dye into the blood vessel to diagnose a blockage, and placement of a stent if appropriate. Bypass surgery involves grafting one or more blood vessels from other parts of the body with the coronary arteries to restore blood flow to the heart.
The average cost of an inpatient admission that included bypass surgery with catheterization (with or without a stent) and major complications was nearly $117,000 in 2018. An admission for a bypass surgery that did not involve catheterization or complications was $75,688 on average.
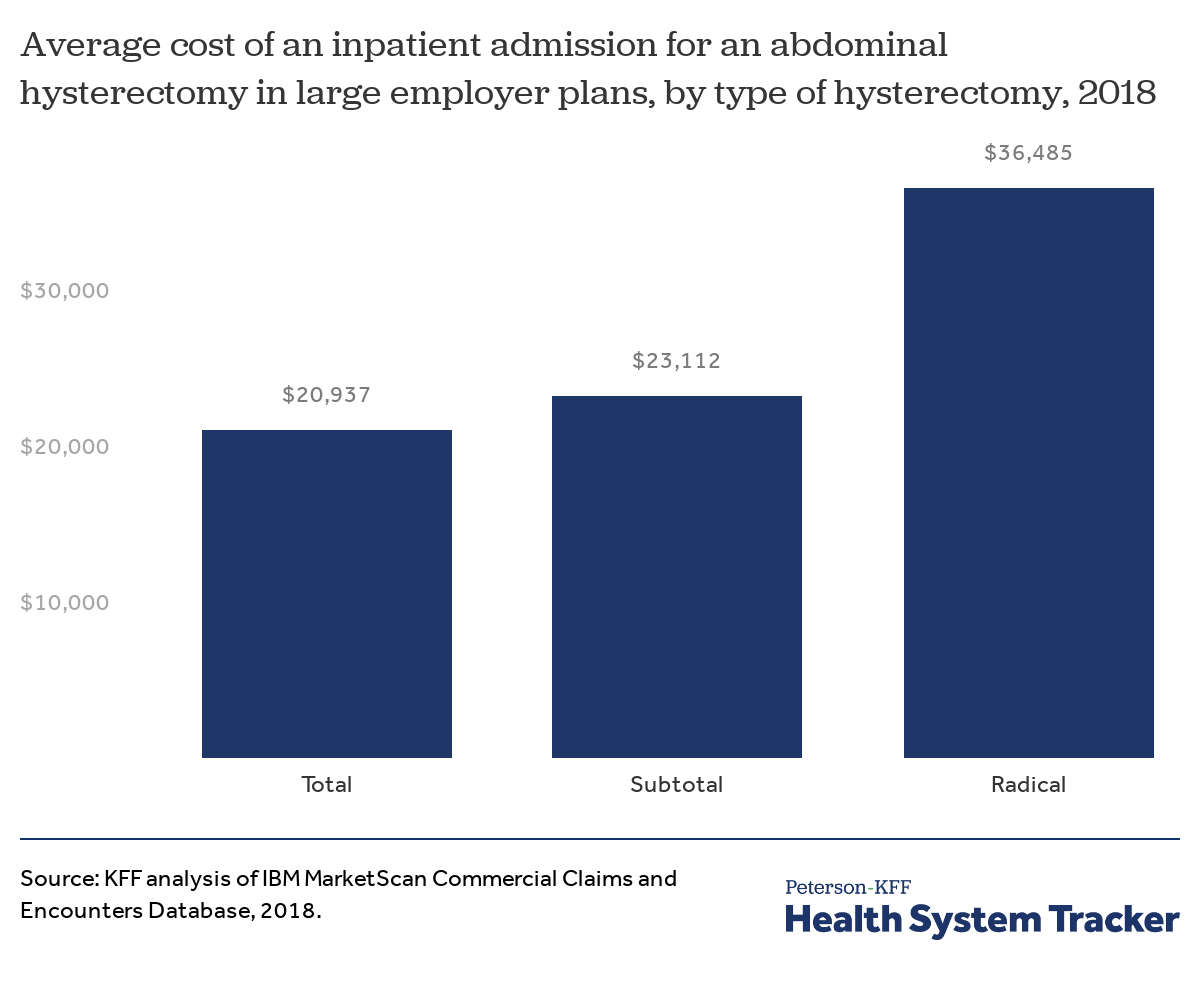
The average cost of an inpatient admission for an abdominal hysterectomy varies by surgical method
Hysterectomy costs vary based on the surgical method used and how much of the uterus and surrounding organs are removed. Most inpatient hysterectomies performed are ‘abdominal’ meaning the surgeon removes the uterus through a larger incision over the belly. This is in contrast to ‘laparoscopic’ and ‘vaginal’ approaches, which refer to performing the operation through smaller incisions in the abdomen or through the vagina, respectively.
Most inpatient hysterectomies are considered total hysterectomies, in which the surgeon removes the whole uterus and cervix. Other kinds include subtotal hysterectomies (removal of only a portion of the uterus leaving the cervix intact) and radical hysterectomies (removal of the whole uterus, the cervix, and the top part of the vagina). Any of these types of hysterectomies could also include the surgical removal of one or both of the fallopian tubes and/or ovaries.
Among large employer plans, the average cost of an inpatient admission for a total abdominal hysterectomy was $20,937 in 2018. Inpatient admissions for abdominal radical hysterectomies were substantially more costly at $36,485 on average, possibly because they are more invasive and because radical hysterectomies are often associated with malignancy and more complex conditions. The following chart shows costs for laparoscopic hysterectomies.
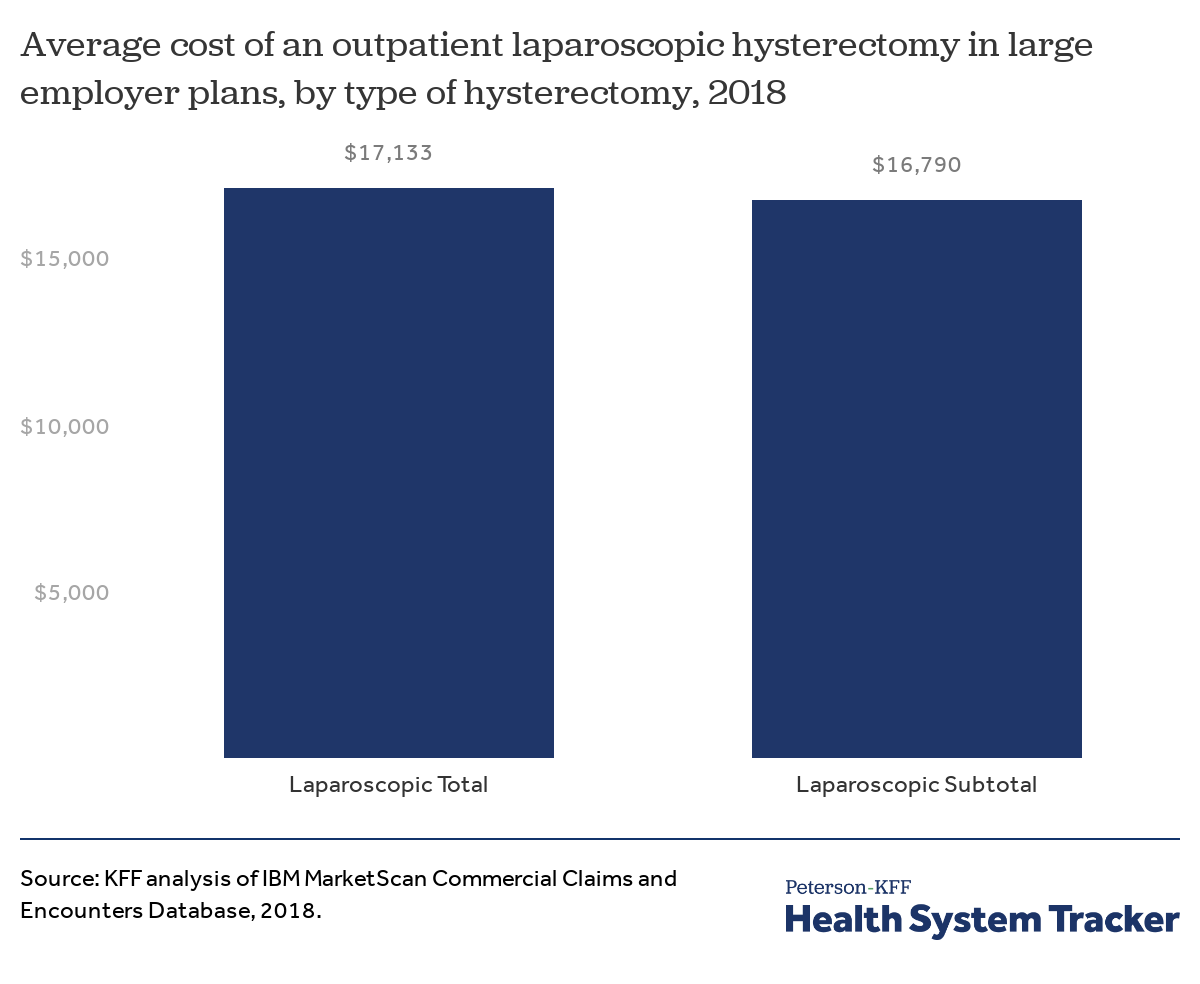
Total and subtotal hysterectomies performed laparoscopically on an outpatient basis are slightly less costly than inpatient abdominal hysterectomies
Laparoscopic hysterectomies are more common in outpatient settings and the cost of these procedures varies less dramatically than inpatient abdominal hysterectomies. On an outpatient basis, the average cost of a subtotal laparoscopic hysterectomy ($16,790) is just $343 less than the average cost of a total laparoscopic hysterectomy ($17,133). Laparoscopic hysterectomies are less invasive and, in most cases, require less recovery time than abdominal hysterectomies. Radical hysterectomies are also less commonly performed in outpatient settings.
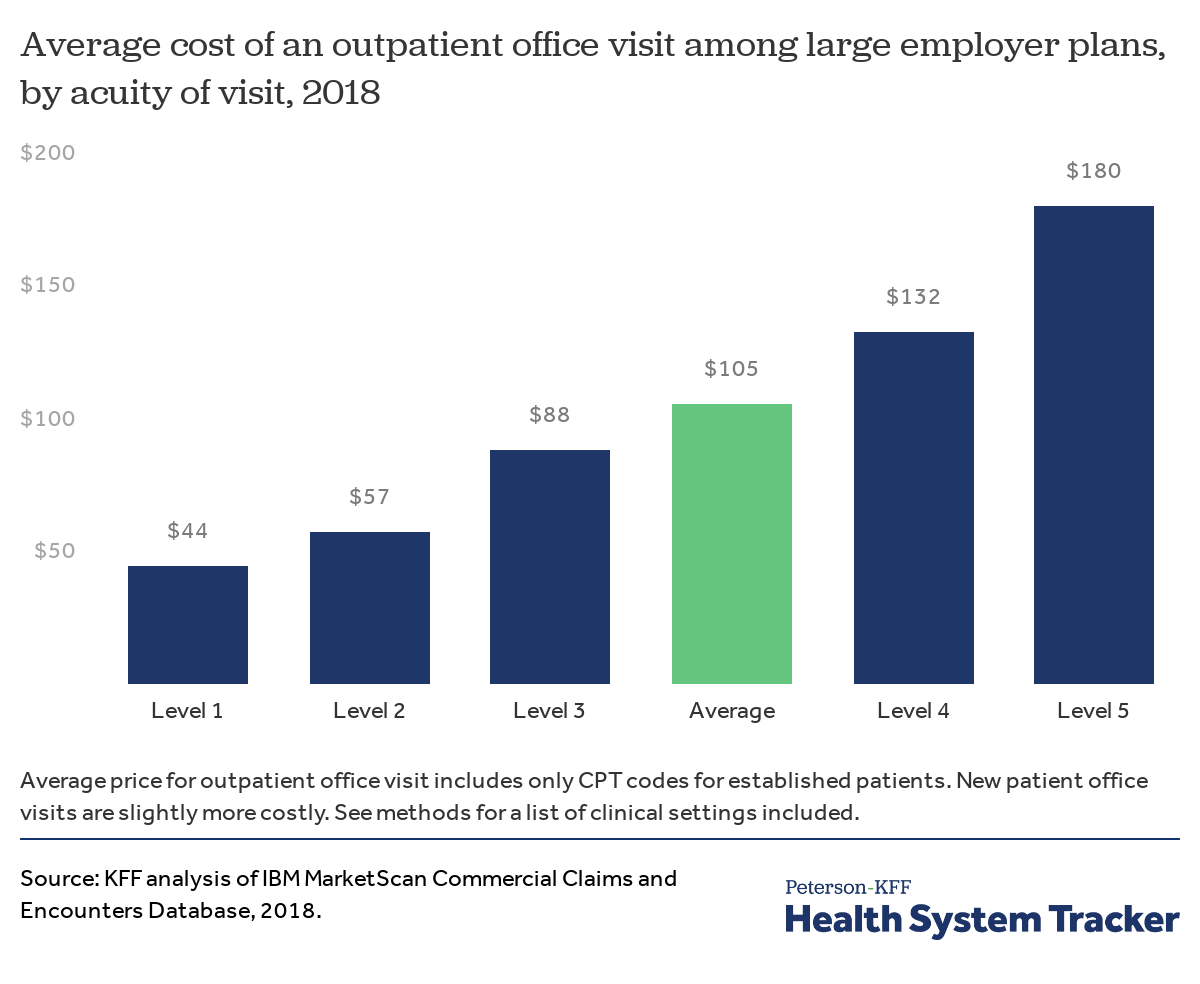
There is considerable variation in the cost of outpatient visits depending on the severity and complexity of the visit
Outpatient physician visits with the highest level of acuity (the most severe and most complex) are coded as Level 5, whereas visits for straightforward, minor conditions are coded as Level 1. Physician visits for the most complex cases (Level 5) cost an average of $182 per visit, while compared to $46 for the simplest visits. The most common physician visits are coded as Level 3, which average $90 per visit. Overall, the average cost of an outpatient visit was $105 in 2018.
The following chart shows how the cost of an office visit has changed over time for each level.
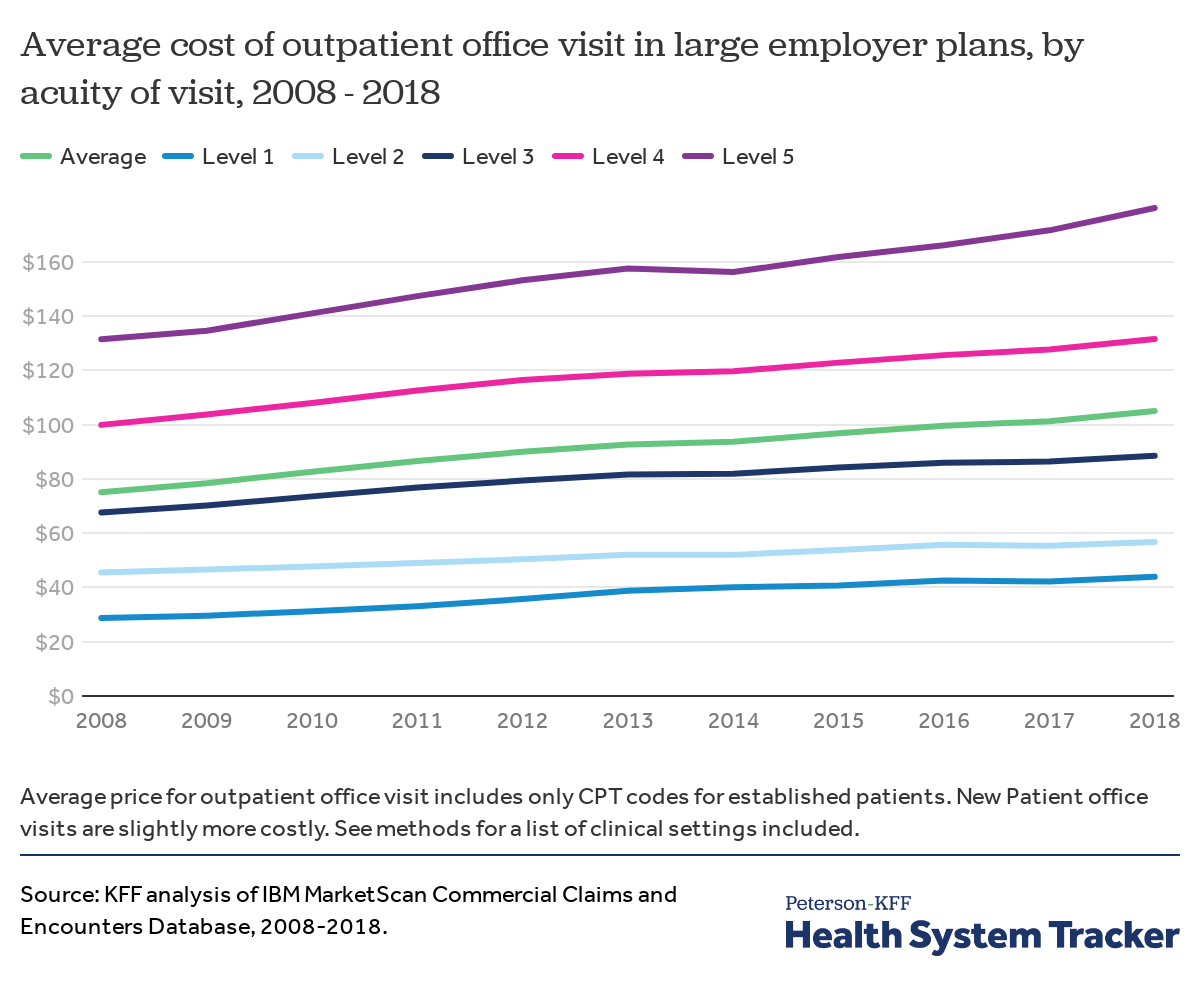
Costs have increased over the past 10 years for all levels of outpatient visits
Average costs have increased for each of the five levels of office visits. From 2008 to 2018, the average cost of Level 1 office visits increased by $15 (or 52%) and the average cost of Level 5 office visits increased by $49 (or 37%). The average cost of Level 3 office visits, by far the most commonly coded severity, rose by $20 (or 29%) over the same period.
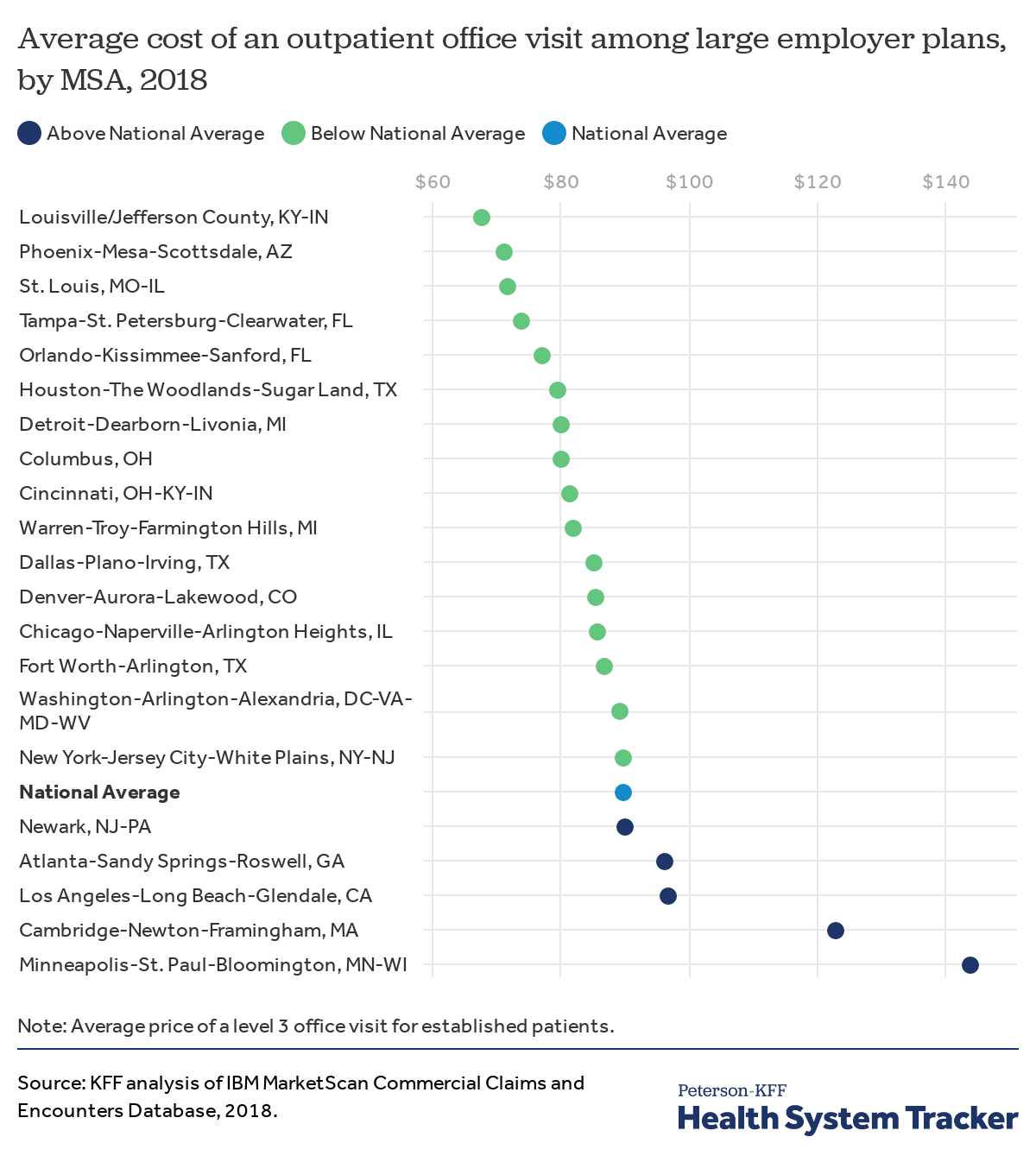
The average cost of outpatient visits varies considerably across markets
This chart shows the variation in the cost of Level 3 outpatient office visits across the largest MSAs with more than 10,000 visits in 2018. As an example, the average office visit in the Minneapolis and St. Paul area ($144) is more than double the average cost in the Louisville area ($68) and 60% higher than the national average ($90).
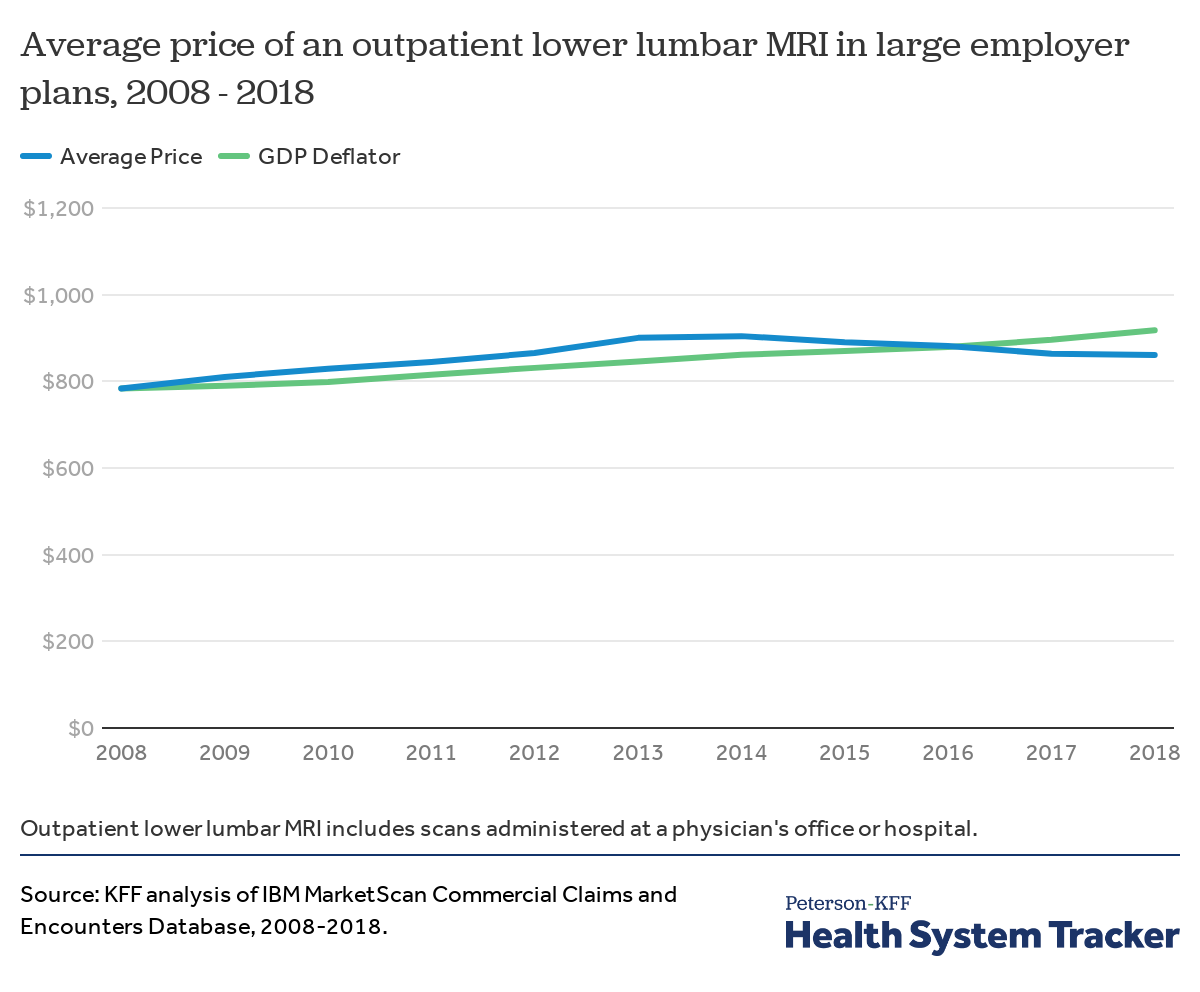
The average price of lower back MRIs has increased slower than inflation
Not all services have experienced rapid increases in prices. In 2018, the average price of an outpatient lower back MRI was $861, up from $784 in 2008. This represents a 9% price increase over 10 years, which was lower than general price inflation over the same period (17%). The prices here include the cost of the MRI itself and the professional cost of the radiologist interpretation.
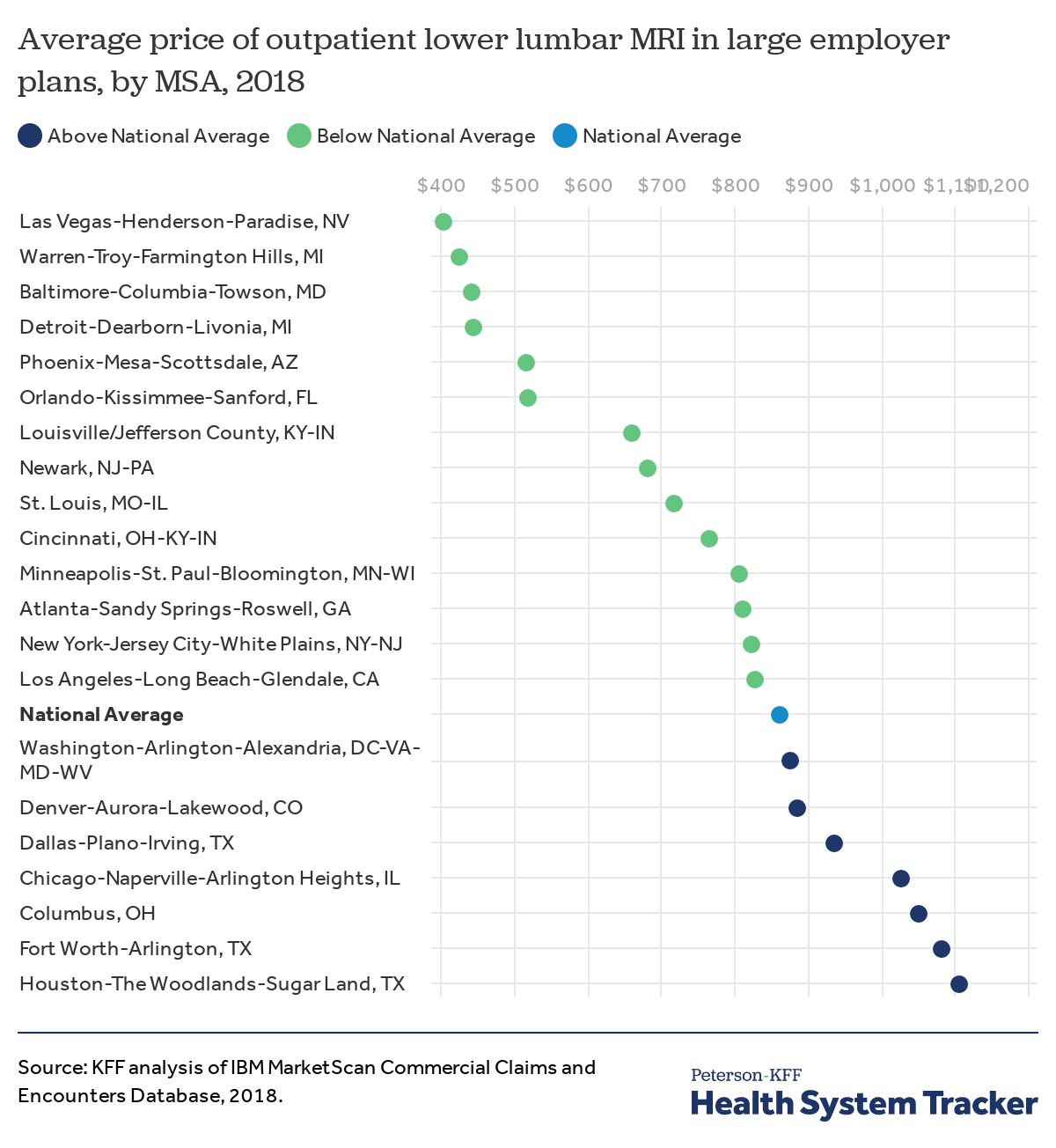
The average price of lower back MRIs varies considerably by location
While the average price of a lower back MRI did not substantial increase from 2008 to 2018, there is large variation in the price of this procedure across the country. The highest average price for a lower back MRI is in the Houston, TX area ($1,106), which is nearly triple the average price in the Las Vegas area ($404), and 32% higher than the national average ($861).
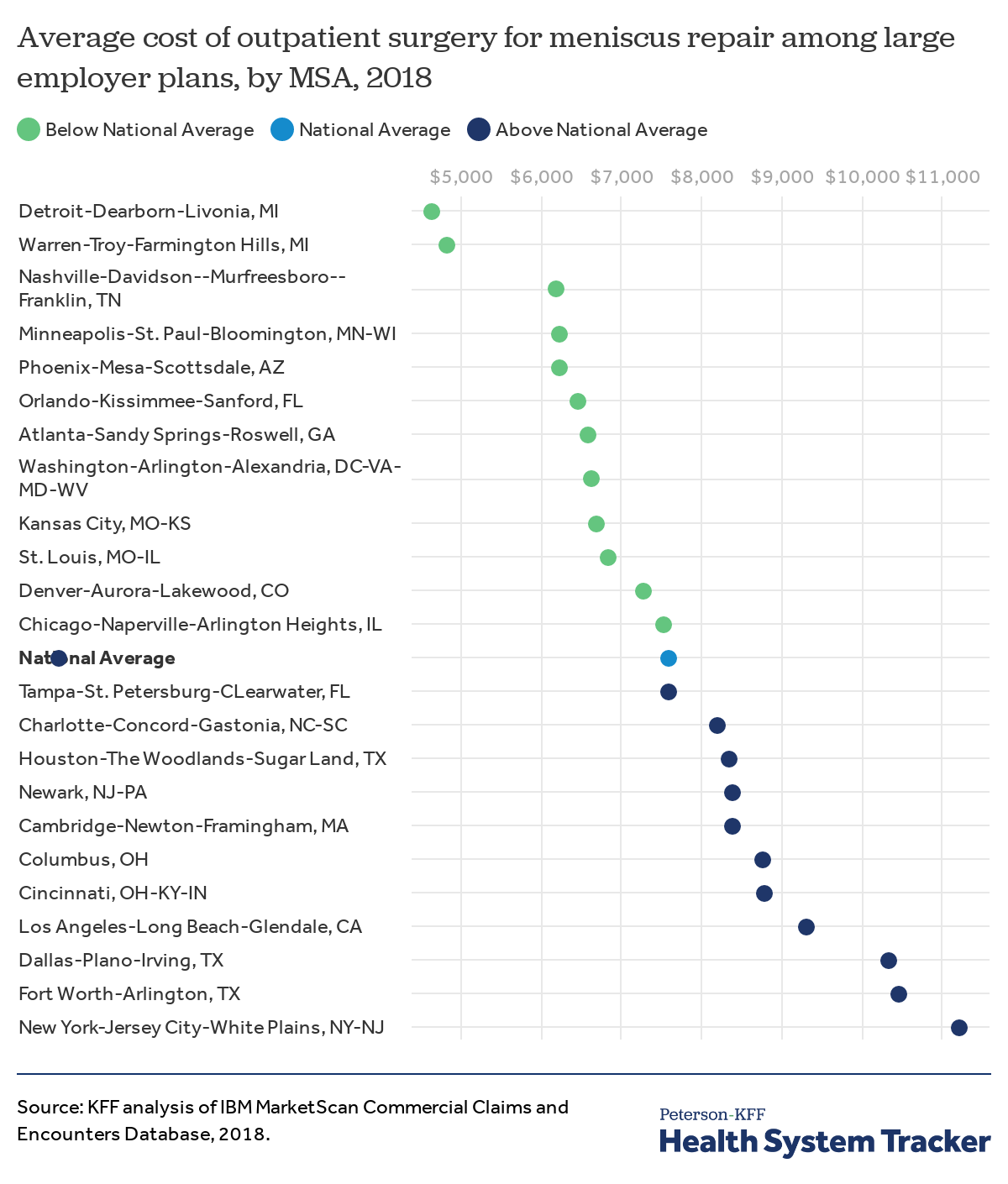
The cost of outpatient surgery to repair torn knee cartilage varies considerably across the country.
Meniscus repair is an outpatient surgical procedure to repair torn knee cartilage. The national average cost for this procedure is $7,595, but there is considerable variation across MSAs. For example, the highest average cost for outpatient meniscus repair surgery is in the NYC area ($11,219), more than double the cost in the Detroit area ($4,655), and 48% higher than the national average.
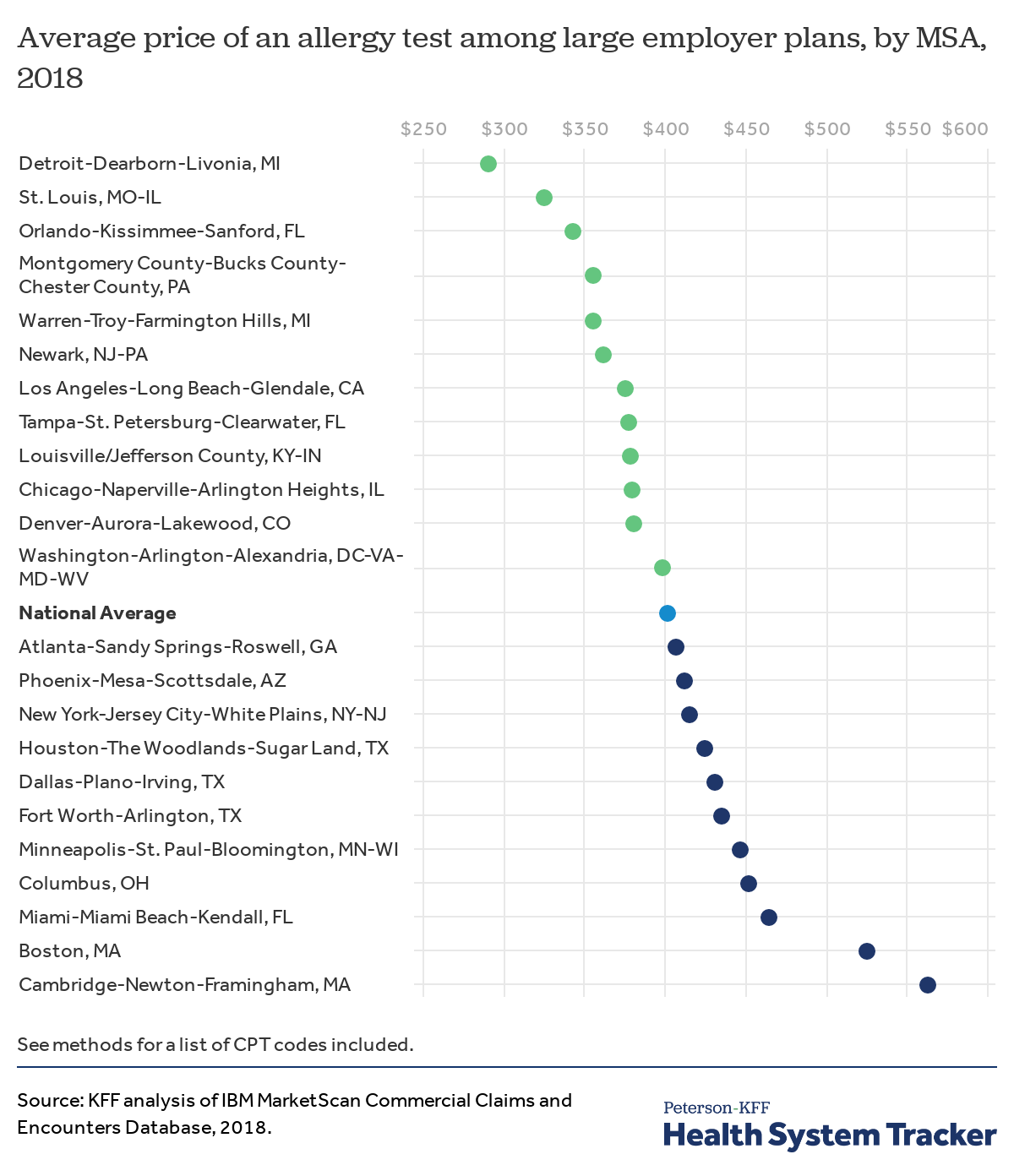
There is considerable variation in the price of an allergy test across the country
The national average cost of an allergy test is $424, but there is a considerable range in prices across geographic areas. The highest average price for an allergy test is in the Cambridge, MA area ($575), which is 76% higher more than the average price in the Detroit area ($326).
Discussion
Although recent policies have attempted to improve the transparency of health prices, a general lack of transparency makes it difficult for enrollees to know the total cost of a procedure or visit in advance, and even more difficult for them to know what their own liability may be. Additionally, many patients inadvertently receive treatment from out-of-network providers, putting them at risk for surprise medical bills. While this analysis examines average costs paid by insurers and enrollees for a number of common services, it also highlights the significant costs people may face for out-of-network providers.
The high cost of inpatient and outpatient care is the primary driver of the difference in health spending between the U.S. and similarly large and wealthy countries. As this analysis shows, even within the U.S., the cost of common health services can vary considerably from city to city (and a related analysis shows how these costs can even vary widely within cities). In some cases, this variation may be due to differences in severity of illness or complexity of service, but in other cases, this variation highlights extremely high and questionable prices set for care.
This analysis also shows that the cost of several health services has increased at a rate faster than general economic inflation – in some cases, many times faster. These rapidly rising costs of health services underlie growing premiums and deductibles for people with employer health insurance. Over the last decade, the amount employees have paid toward their premiums and out-of-pocket costs has exceeded wages, meaning that health care costs – and other expenses – have become harder to afford, even for those with relatively generous health coverage.
Methods
We analyzed a sample of claims obtained from the Truven Health Analytics MarketScan Commercial Claims and Encounters Database (MarketScan). The database has claims provided by large employers (those with more than 1,000 employees). This analysis only includes costs for services covered by large employer plans. We used a subset of claims from the years 2008 through 2018. In 2018, there were claims for almost 18 million people representing about 22% of the 82 million people in the large group market.
Weights were applied to match counts in the Current Population Survey for large group enrollees by sex, age, state and whether the enrollee was a policy holder or dependent. People 65 and over were excluded. We also limited claims to fee-for-service claims (excluding claims collected on an encounter basis). For all inpatient admissions, we excluded the top 0.5% of claims and claims that fall below either $5,000 or 10% of the average total price off the service, whichever is lower. For outpatient services or procedures, we also exclude the top 0.5% of claims and, unless otherwise specified below, claims that fall below either $5 or 10% of the average total price of the service, whichever is lower.
When showing the cost of a common service over time, we use the GDP deflator to benchmark the change in the price of the specific service against the change of prices in the general economy. The GDP deflator is a measure of inflation that captures the prices of all new, domestically produced goods and services. For charts depicting variation in the cost of a common service across Metropolitan Statistical Areas (MSAs), we select the 25 most populous MSAs with more than 125 procedures (unless otherwise specified in the text).
Midway through 2015, MarketScan claims transitioned from ICD-9 to ICD-10. While both systems classify procedures, they do not precisely crosswalk. Below is a summary of which codes we included:
- The cost of an inpatient admission for total knee or hip replacements are the cost of all services associated with an inpatient admission in which the principal procedure was ICD-9 code 81.54 or any of the subsequent procedures under the ICD-10 headings 0SRD and 0SRC. In addition, admissions without a principal procedure but in which the claim includes CPT code 27447 are included.
- The cost of an inpatient admission for a laparoscopic appendectomy is the cost of all services associated with an inpatient admission in which the principal procedure was ICD-9 code 47.01 or ICD-10 code 0DTJ4ZZ.
- The cost of an inpatient admission for a laparoscopic cholecystectomy is the cost of all services associated with an inpatient admission in which the principal procedure was ICD-9 codes 51.21- 51.24, or ICD-10 codes 0FB44ZZ, 0FT44ZZ, 0FT40ZZ, or 0FB40ZZ.
- The cost of an inpatient admission that include a heart attack is the cost of all services associated with an inpatient admission where the patient received one of the following ICD-10 codes: I2101, I2102, I2109, I2111, I2119, I2121, I2129, I213, I214, I220, I221, I222, I228 or I229.
- The cost of an inpatient admission for Coronary Artery Bypass Graft (CABG) surgery is the cost of all services associated with an inpatient admission where the associated diagnosis-related group (DRG) was 233, 235, or 236.
- The cost of an inpatient admission for an abdominal hysterectomy is the cost of all services associated with an inpatient admission where the admission includes CPT code 58150, 58152, 58180, or 58210.
- The cost of outpatient meniscus repair is the cost of all services on a day that contains the following: a diagnosis code under the ICD-10 headings S83.2 or M23 (meniscus injury), CPT code 29880 or 29881 (arthroscopy on knee), CPT code 01400 (anesthesia for knee surgery), and occurred in an ambulatory surgical center or in a hospital on an outpatient basis.
- The cost of an outpatient laparoscopic hysterectomy is the cost of all services on a day in which the primary procedure was CPT code 58570-58575 (total) or 58541-58544 (subtotal).
- The cost of outpatient lower lumbar MRIs includes the cost of outpatient claims with a CPT code of 72148. In addition to claims for professional services, some claims include facility fees. In cases in which no other professional services are provided on the date of service, facility fees were included in the cost of the MRI. In order to ensure that we are capturing the cost of performing the MRI and not associated services, claims in which all the cost in a day have a procedure modifier 26 are excluded.
- The cost of an outpatient office visit is the weighted average of the cost of CPT codes 99211, 99212, 99213, 99214 and 99215. These visit codes are for established patients but vary in complexity and duration. Claims with a total cost less than $5 were excluded.
- The cost of an allergy test is the weighted average cost of CPT codes corresponding with common skin tests: 95024, 95004, 95018, 95027, 95017, 95028, and 83520. Claims with a total cost less than $5 were excluded.
The Peterson Center on Healthcare and KFF are partnering to monitor how well the U.S. healthcare system is performing in terms of quality and cost.