In addition to its devastating health toll, COVID-19 can also lead to significant financial costs for people needing treatment and for public and private payers. In this chart collection, we examine the cost of COVID-19 treatment for inpatient care among people with health coverage through large employers.
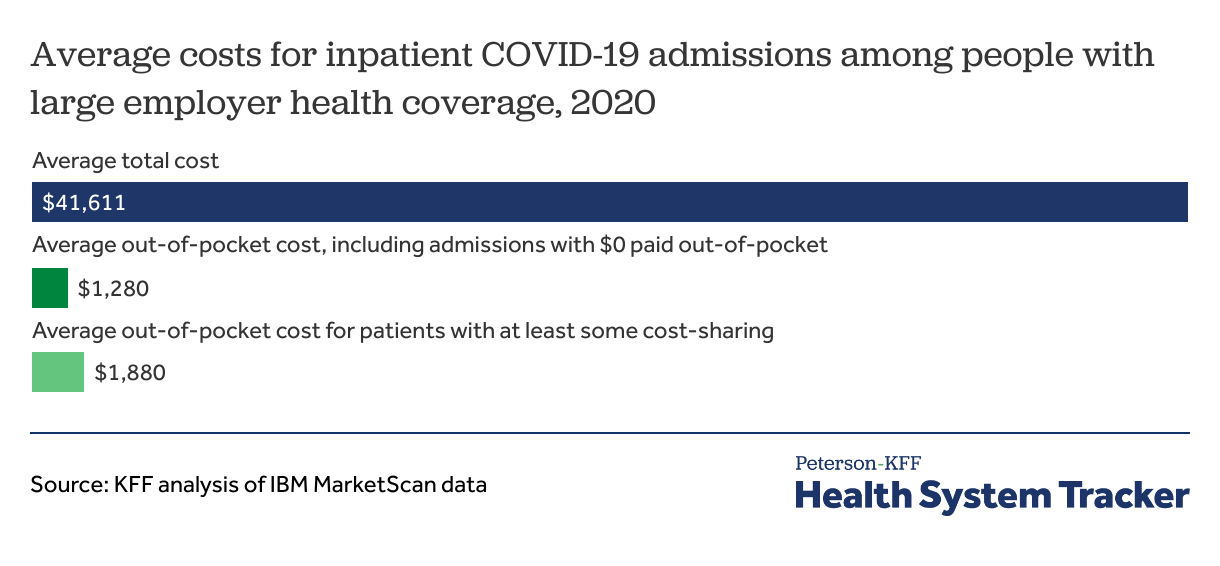
We find that, in 2020, COVID-19 hospitalizations cost an average of $41,611, including an average out-of-pocket payment of $1,280 for people with large employer coverage. In 2020, many private insurers and employers temporarily waived out-of-pocket costs for COVID-19 treatment (this is generally no longer the case). For COVID-19 hospitalizations with some cost-sharing expense, an average of $1,880 was spent out-of-pocket by individuals with large employer coverage.
As we show in the following charts, COVID-19 hospitalization costs vary widely for patients with private insurance. This analysis focuses on people with large employer coverage and does not reflect costs for patients with Medicaid or Medicare. At this time, 2020 is the most recent year of available data, and hospitalization and other treatment costs may have changed with the introduction of newer treatments.
On average, COVID-19 hospitalizations cost over $41,000 for people with large employer coverage
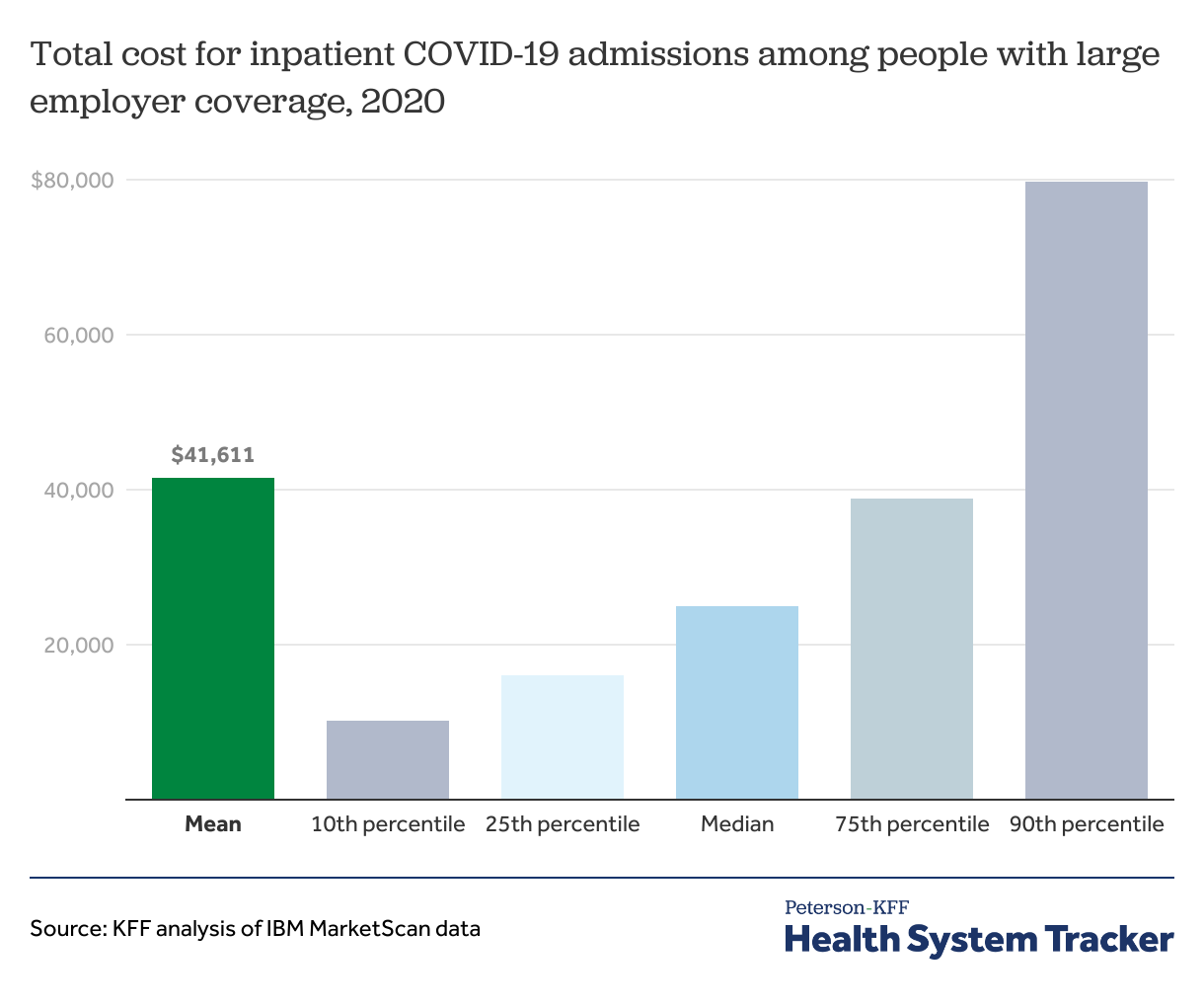
In the chart above, we examined the average amount paid for COVID-19 hospital admissions in 2020. On average, the amount paid by the plan and the enrollee combined totaled $41,611.
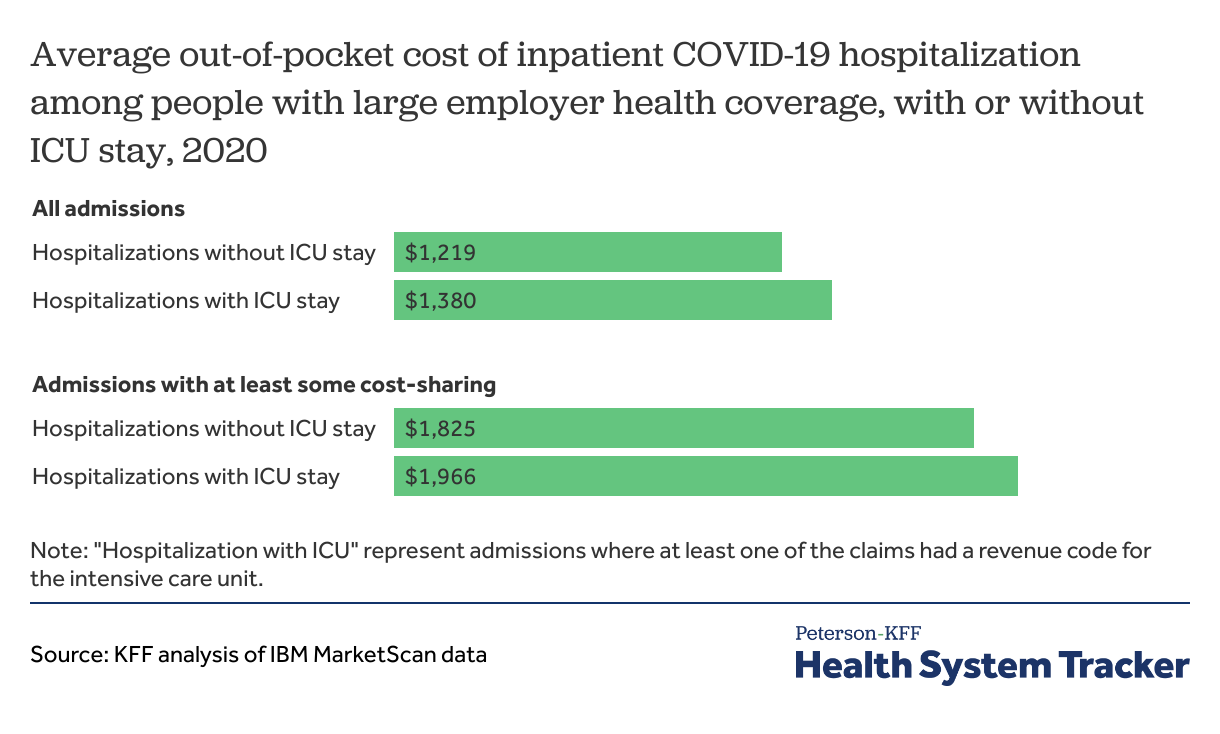
The average out-of-pocket cost associated with a COVID-19 hospitalization was $1,280 in 2020. However, many insurers temporarily waived out-of-pocket costs in 2020 and most had stopped waiving these costs by late 2021. As a result, this average (which includes many hospitalizations with $0 in out-of-pocket costs) may not be an accurate representation of the typical out-of-pocket liability patients experience today. Out-of-pocket average costs for inpatient COVID-19 treatment in 2021 and 2022 are likely to be higher than in 2020, as these voluntary waivers became uncommon.
Looking only at admissions with at least some out-of-pocket spending, the average out-of-pocket spending was $1,880. (Note that some patients may pay $0 out-of-pocket due to COVID-19 specific cost-sharing waivers, while some may have already met a plan deductible or out-of-pocket limit.)
The mean cost of a COVID-19 hospitalization in 2020 was over $41,000. Patients paid an average of $1,280 out of pocket per admission. Share on XCosts for COVID-19 hospitalizations can vary widely
In general, hospitalization costs can vary widely based on factors such as severity and prices, and COVID-19 is no exception.
Among people with large employer-based health coverage, half of COVID-19 hospitalizations in 2020 cost over $25,000 and a quarter cost over $38,000. The exceptionally high-cost cases bring the average cost to above $40,000. As shown below, hospitalizations that include a stay in intensive care (ICU) are significantly more expensive than those that do not.
Out-of-pocket costs for COVID-19 hospitalizations can vary widely
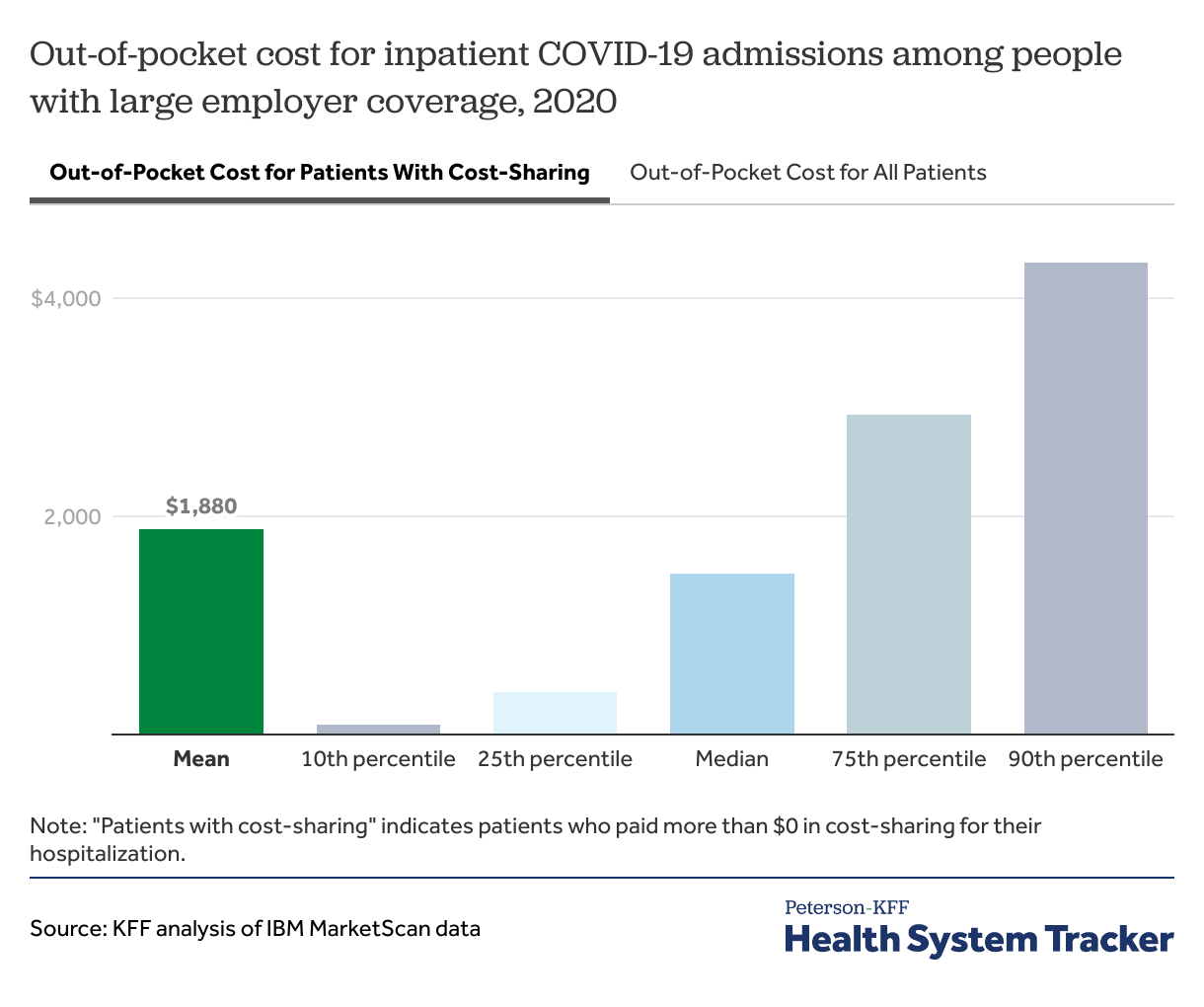
In 2020, many insurers and employers waived out-of-pocket costs for COVID-19 treatment. Still, we find 68% of COVID-19 admissions in 2020 had at least some out-of-pocket costs.
Among COVID-19 hospitalizations with cost sharing, half had out-of-pocket costs over $1,470, and a quarter had out-of-pocket costs exceeding $2,900.
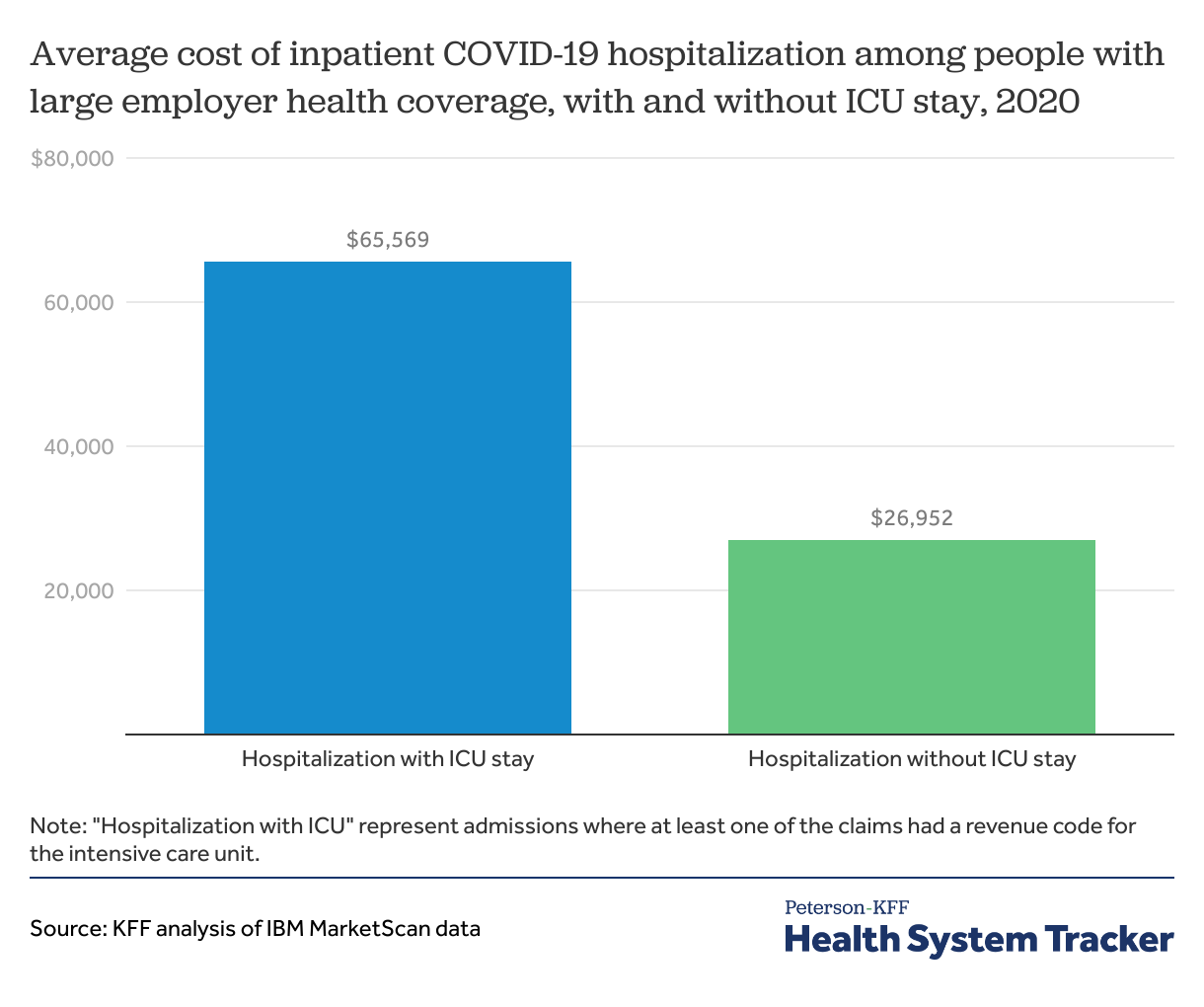
COVID-19 admissions with intensive care are more than double the cost of those without an ICU stay
About 38% of COVID-19 hospitalizations in 2020 among people with large employer-sponsored insurance included an intensive care unit (ICU) stay in 2020. Among COVID-19 admissions with ICU treatment, the average cost was $65,569, more than double that for COVID-19 admissions without intensive care ($26,952).
COVID-19 ICU stays in 2020 were more costly on average than other ICU stays. Among other patients who required ICU care but did not have COVID-19, the average hospitalization for people with large employer-sponsored insurance cost $49,560.
Out-of-pocket cost for COVID-19 admissions with or without ICU stay was similar for people with large employer coverage
While ICU admissions more than twice as expensive on average as admissions without intensive care, the amount paid by patients out-of-pocket was similar (likely because patients admitted to the hospital tend to reach their deductible or out-of-pocket maximum). Average out-of-pocket costs for an ICU hospitalization was $1,380, while for a hospitalization without an ICU stay it was $1,219. However, ICU patients with at least some cost-sharing had higher out-of-pocket costs for ICU COVID-19 admissions, averaging $1,966.
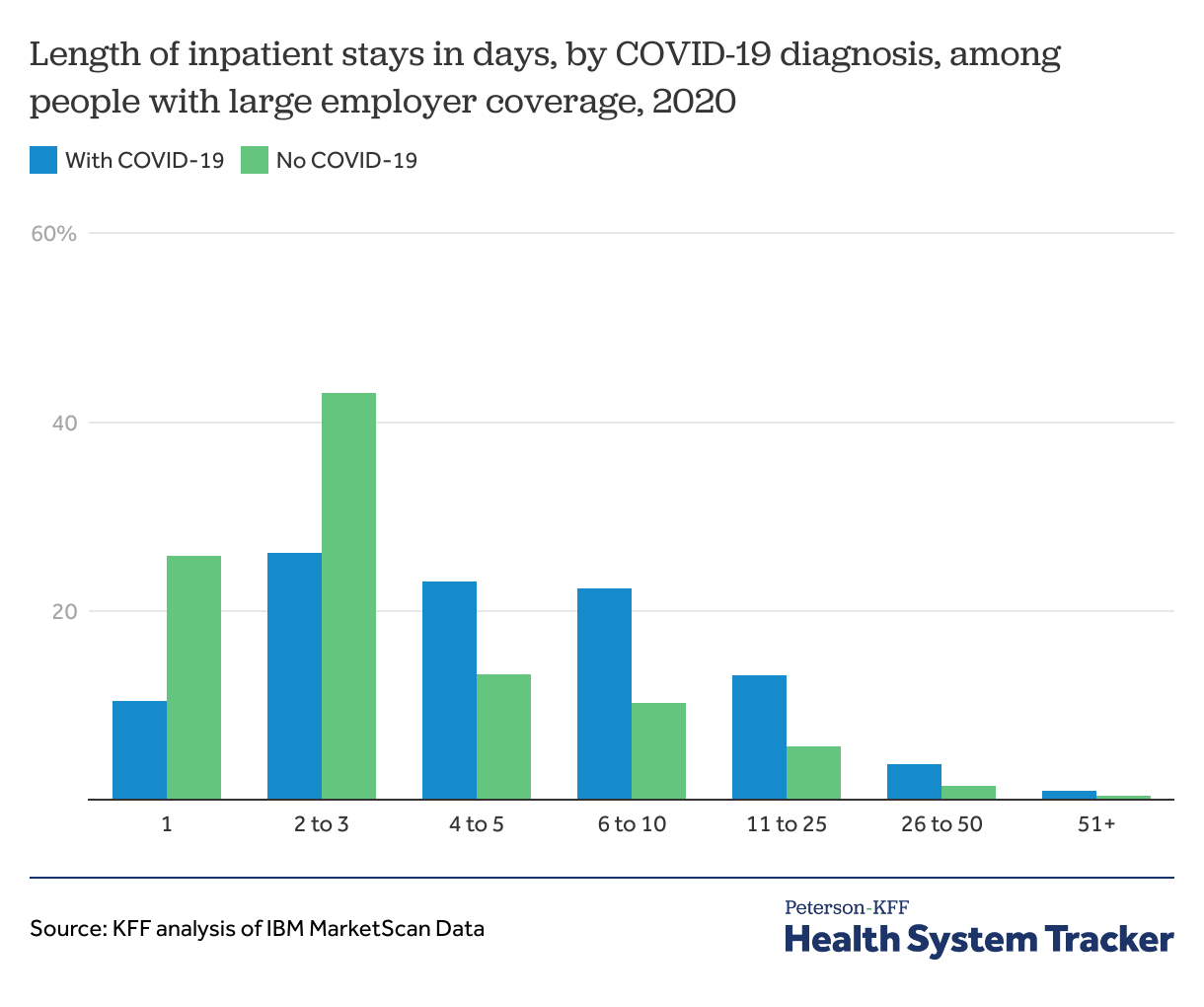
COVID-19 hospital admissions were longer than other hospitalizations, on average
COVID-19 admissions were longer than other admissions, with an average COVID-19 admission lasting 7 days compared to 4 days for other admissions.
Discussion
The total cost of inpatient treatment for COVID-19 for individuals with large employer coverage averaged over $40,000, and patient out-of-pocket costs commonly exceeded $1,000. In 2020, some individuals received cost-sharing waivers and were not liable for any out-of-pocket costs associated with their COVID-19 treatment. However, most hospitalized patients with large employer coverage were responsible for at least some out-of-pocket payments, and these payments frequently exceeded one thousand dollars. Among privately insured non-elderly households in 2019, 21% of single-person households and 13% of multi-person households had liquid assets of less than $1,000. This can lead to financial hardship and difficulty covering the cost of a COVID-19 hospitalization, despite the patient’s insured status.
Most of the total cost of COVID-19 treatment is covered by an insurer if the patient’s employer is fully insured, or the employer itself if it is self-insured. This may put upward pressure on premiums in future years, affecting all enrollees, regardless of whether they had a COVID-19 hospitalization. However, the pandemic also saw a decrease in patients seeking other forms of care, including elective procedures. Insurers generally expected the pandemic to have a small effect on premiums in 2023.
Methods
We used 2020 MarketScan inpatient data. COVID-19 hospital admission was identified if test confirmed COVID-19 diagnosis or a diagnosis related to COVID-19 encounter (pneumonia, acute bronchitis, lower respiratory infection, acute respiratory distress syndrome) was present on the admission day. The Centers for Disease Control and Prevention (CDC) announced COVID-19 coding guidance in February 2020 prior to establishing a COVID-19 ICD-10 diagnosis code in early April 2020. We used the coding guidance and the ICD-10 diagnosis U07.1 code to identify COVID-19 hospital admissions. Enrollee claims were trimmed at top 99.5th percentile of total costs and 10% of the bottom 50th percentile of total costs. Average total and out-of-pocket costs were summed for the admission.
MarketScan data were weighted to be representative of enrollees with large employer health plans (employers with a thousand or more workers). Weights were applied to match counts in the Current Population Survey for enrollees at firms of a thousand or more workers by sex, age, state, and whether the enrollee was a policy holder or dependent. Weights were trimmed at eight times the interquartile range.
The Peterson Center on Healthcare and KFF are partnering to monitor how well the U.S. healthcare system is performing in terms of quality and cost.