In this collection of charts, we use a variety of data sources to explore trends in health outcomes, quality of care, and spending on treatment for people in the U.S. with diabetes and other endocrine disorders. In the U.S., diabetes is the most common endocrine disease and is associated with severe health complications such as vision loss, kidney failure, lower-extremity amputations, and heart disease. As the following charts show, the U.S. has seen a reduction in complications due to diabetes and improvement in disease management, but diagnosis rates and diabetes-related spending continue to grow.
Total health spending and out-of-pocket costs are generally higher for people with diabetes than those without diabetes. Recently, the increasing price of some types of insulin has drawn attention from both consumers and lawmakers concerned about insulin affordability for those who rely on it to survive. Complete data regarding these price changes — including discounts drug makers give to insurers and pharmacy benefits managers — are not publicly available. However, it is likely that increases in net prices are lower than increases in list prices after accounting for these discounts. How changes in pricing affect people with diabetes depends on their source of coverage and plan design.
Prevalence and Mortality
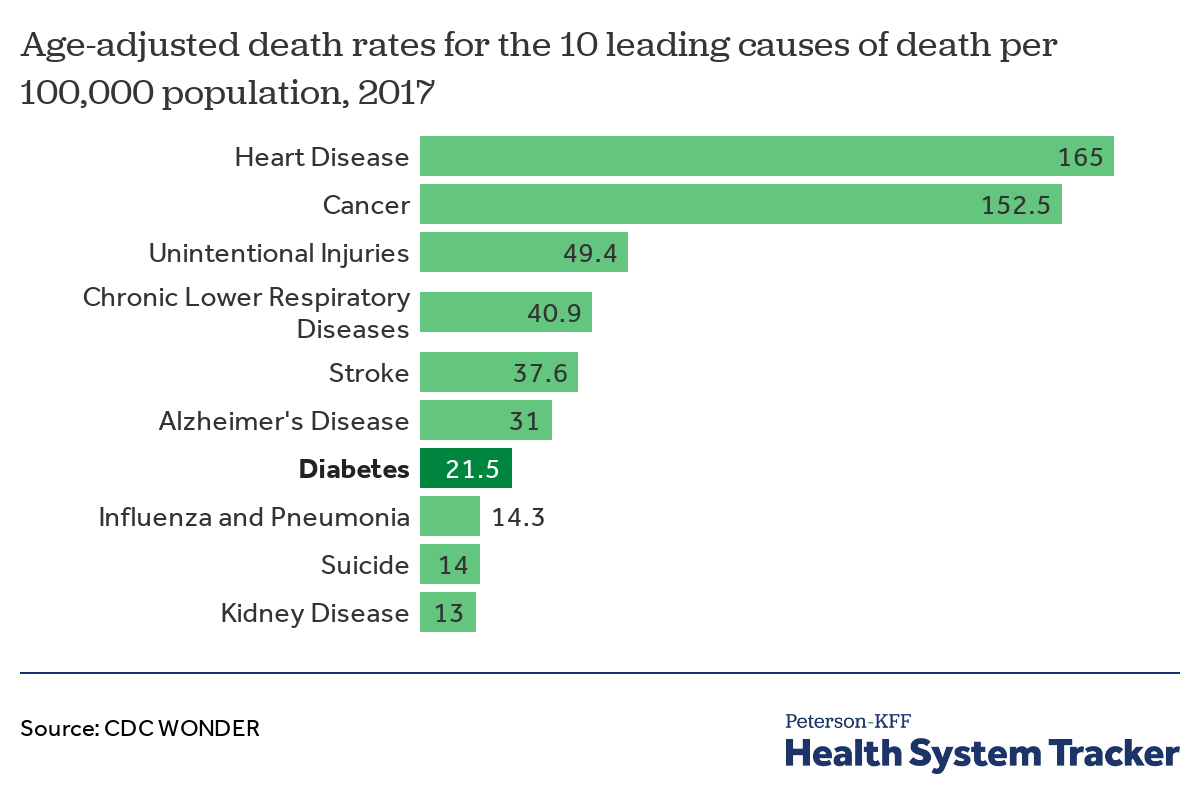
Diabetes is the seventh leading cause of death in the United States
Diabetes is among the 10 leading causes of death in the U.S. Diabetes is a type of endocrine disease. Such diseases occur when any of the major glands in the endocrine system produce too little or too much of a particular hormone, or when the body responds irregularly to hormones. Diabetes, in particular, presents when the body is unable to properly regulate blood sugar levels.
There are three main types of diabetes: type 1, type 2, and gestational diabetes.
- Type 1 diabetes – formerly called juvenile diabetes – is usually diagnosed in children and young adults when the body does not produce insulin. There is no way to prevent type 1 diabetes, and required management includes daily injections of insulin and monitoring blood glucose levels.
- Type 2 diabetes is the most common diabetes diagnosis, accounting for about 90 to 95% of diagnosed diabetes in adults. It occurs when the body in unable to manage insulin properly, causing blood glucose levels to rise.
- Gestational diabetes develops during pregnancy and can present complications for both the woman and child. According to the Centers for Disease Control and Prevention (CDC), gestational diabetes occurs in 6% of pregnancies.
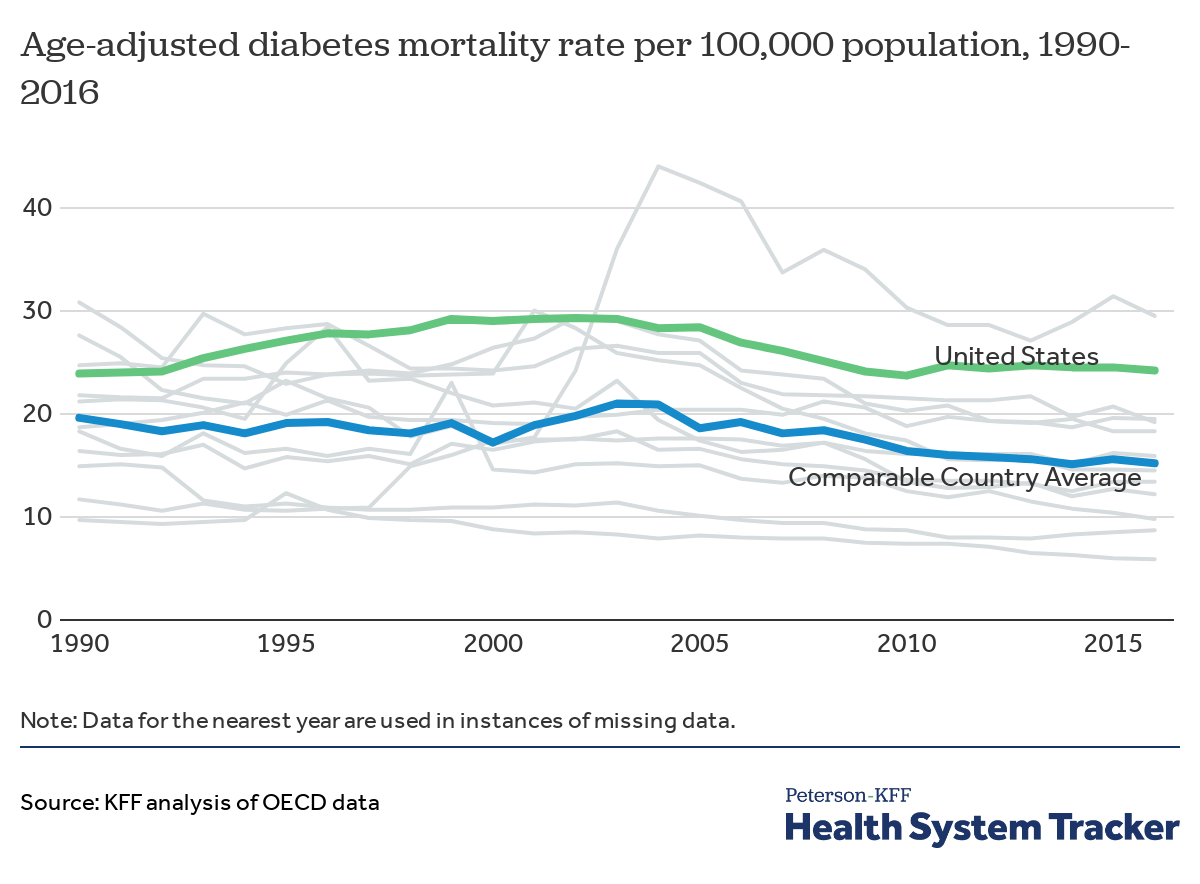
The mortality rate for diabetes in the U.S. remains higher than the average rate for other comparable countries
The diabetes mortality rate in the U.S. rose by nearly 23% – from 23.9 to 29.3 deaths per 100,000 – between 1990 and 2002 and then decreased by 19% to 23.7 per 100,000 by 2010. Between 2010 and 2016, however, the U.S. mortality rate stopped declining and stayed around 24 deaths per 100,000 population. Meanwhile, in similarly wealthy countries, diabetes mortality decreased an average of 22% – from 19.6 to 15.2 deaths per 100,000 – between 1990 and 2016. Austria in particular has higher than average rates of diabetes, which may contribute to the country’s diabetes mortality rate.
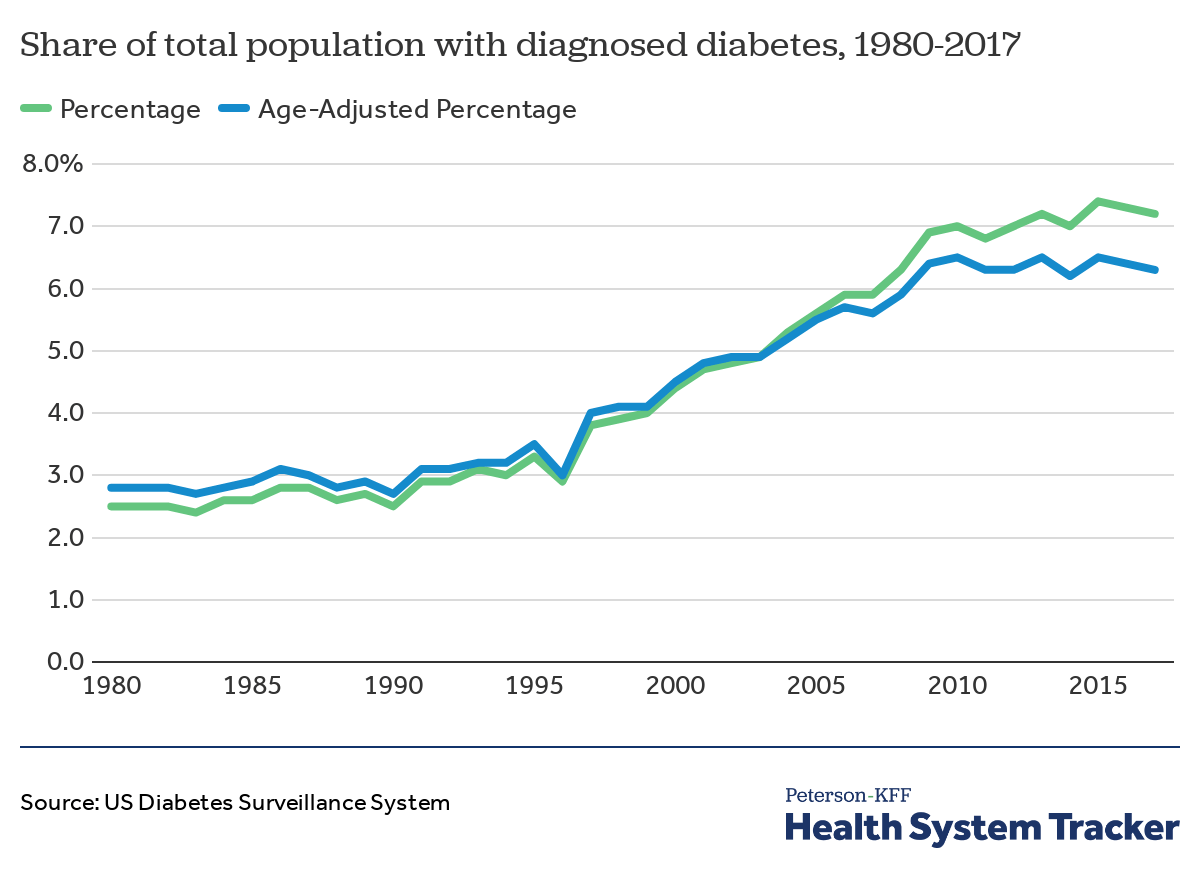
The share of the total population diagnosed with diabetes has been increasing
In 2017, 7.2% of the population was diagnosed with diabetes, or 6.3% of the population when adjusted for age, which takes into account changes in age distribution. This marks a 188% increase from 1980 (and 125% when adjusted for age). Additionally, people who have diabetes may be undiagnosed for the condition. Current estimates from the CDC suggest that 30.3 million people in the U.S. (9.4% of the total population) have diabetes, including 23.1 million with a diagnosis and 7.2 million who are undiagnosed.
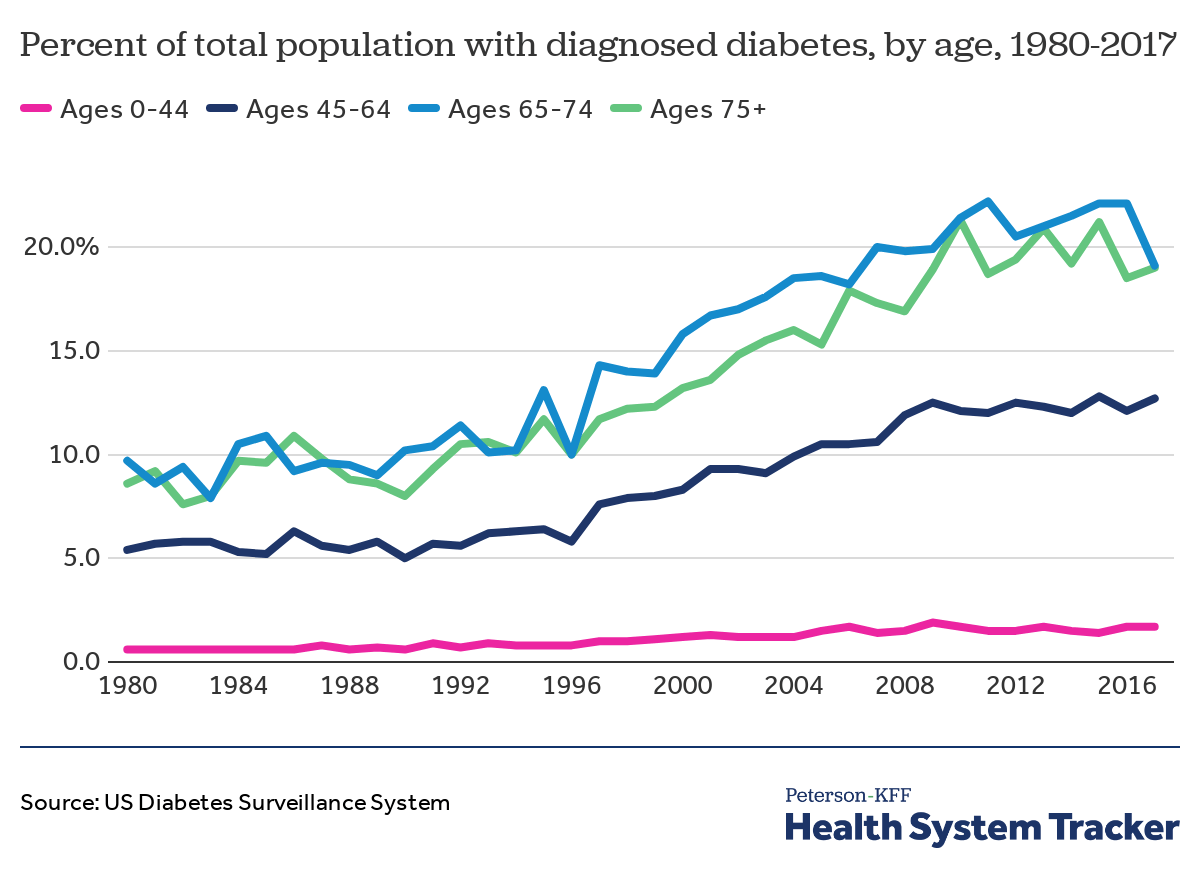
Diabetes diagnoses are more common among people ages 45 or older compared to younger populations
In the U.S., diagnosed diabetes is most common among people ages 65 and older. From 1980 to 2017, there was an overall increase in the share of people with a diabetes diagnoses across all age groups. Although diabetes is less common at younger ages, the share of those 44 years old or younger with a diabetes diagnosis increased slightly between 1980 and 2017.
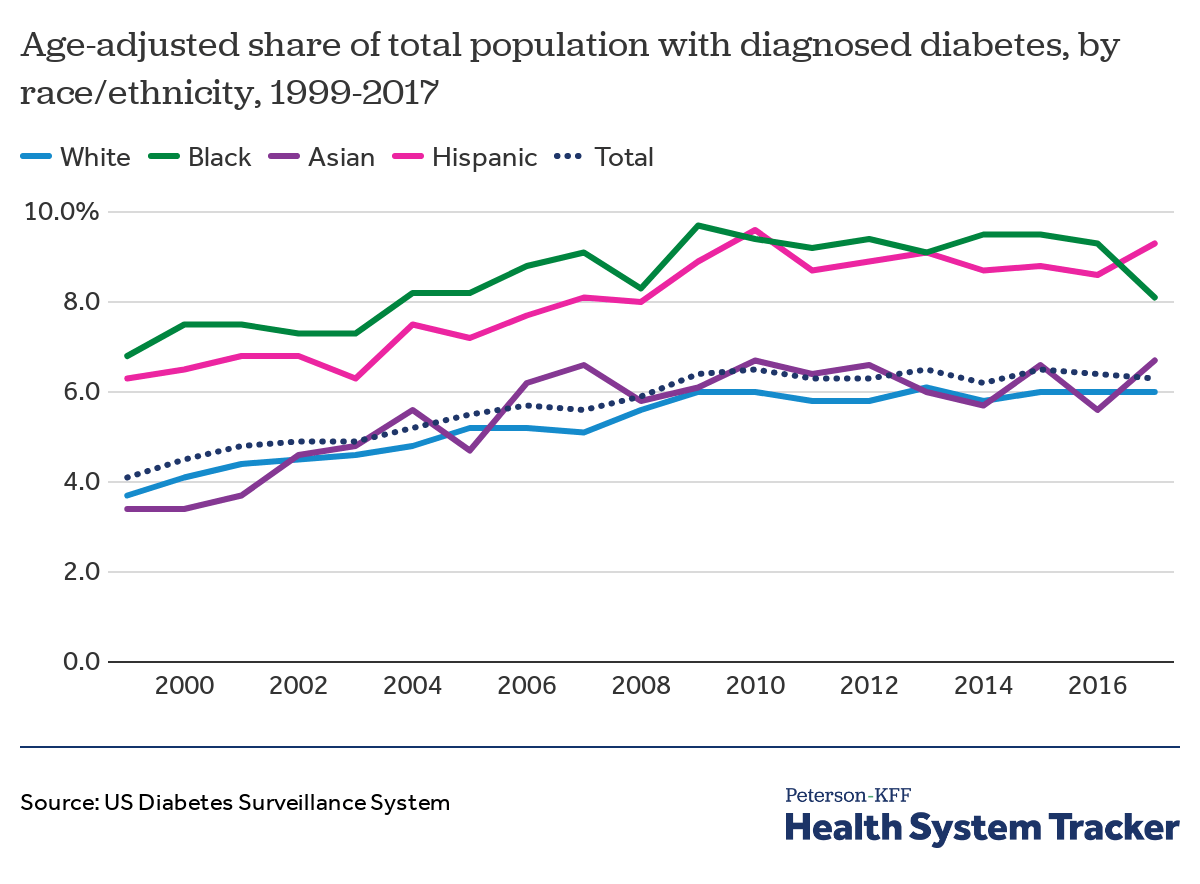
Black and Hispanic people have consistently experienced higher than average rates of diagnosed diabetes
In the U.S., the prevalence of diabetes has increased over time across all racial and ethnic groups and most rapidly among Asian and White people, but Black and Hispanic people continue to have the highest rates of diagnosed diabetes. In 2017, 6% of White people and nearly 7% of Asian people had a diabetes diagnosis, compared to over 8% of Black people and over 9% of Hispanic people — well above the national average of 6% of the total population for all ages. From 1999 to 2017, the percentage of people with a diabetes diagnosis increased by 19% among Black people, 48% among Hispanic people, 62% among White people, and 97% among Asian people.
Affordability
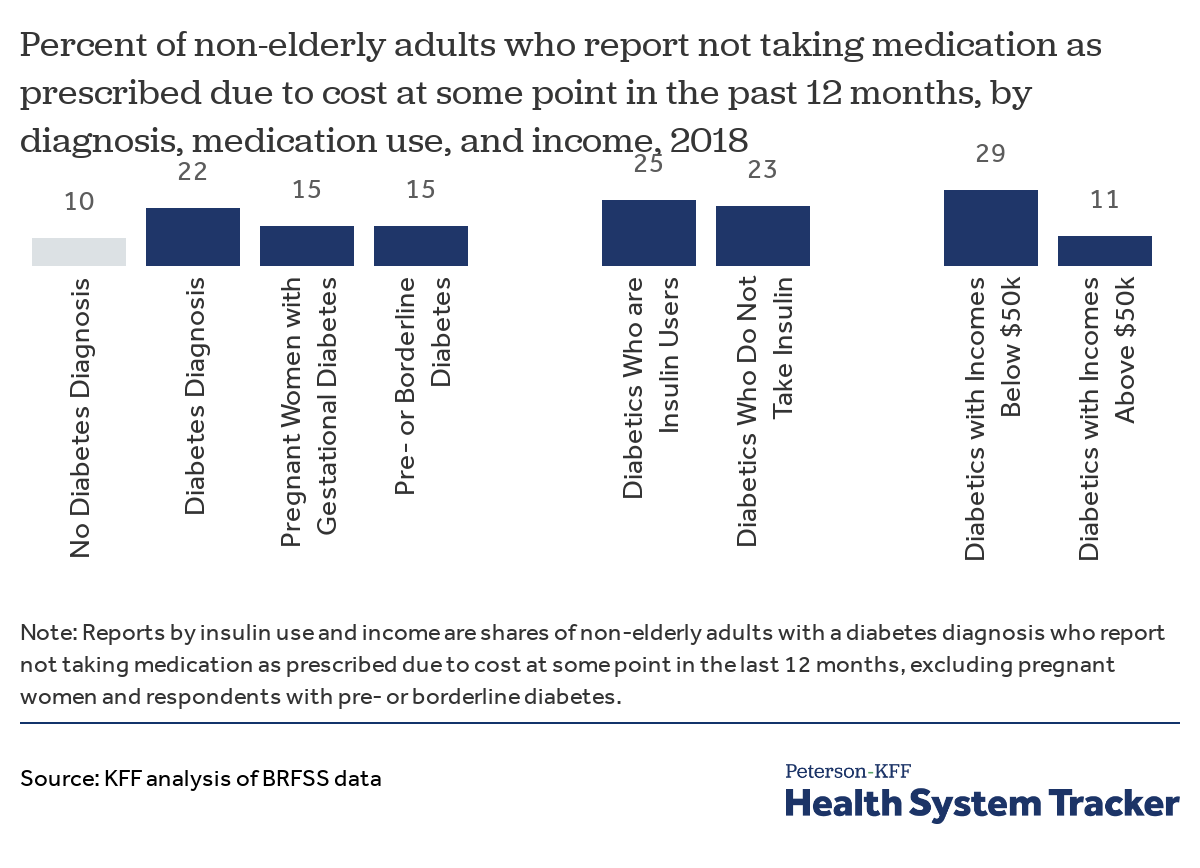
Adults with diabetes are more likely to report cost as a barrier to taking medication as prescribed
About 1 in 5 (22%) of non-elderly adults with a diabetes diagnosis reported not taking medication in advance due to cost, compared to 1 in 10 (10%) adults without a diabetes diagnosis, and 15% of adults with pre- or borderline diabetes. Out of those with a diabetes diagnosis, lower-income adults (income below $50,000 per year) were more than twice as likely to report not taking medications as prescribed due to cost, compared with adults with incomes above $50,000 per year (29% vs. 11%). Similar shares of diabetics who take insulin and those who do not take insulin reported that cost was a barrier to taking medication as prescribed (25% and 23%, respectively).
Diabetes is commonly treated with medication, which includes insulin injections and oral medication, among other treatment options. According to the CDC, while most adults with a diabetes diagnosis (81%) reported using either insulin or pills for diabetes management in 2016, nearly 1 in 5 adults with diabetes (19%) reported not using any diabetes medication. Additionally, nearly 1 in 4 (24.4%) adults with diabetes asked their doctor for a lower-cost medication.
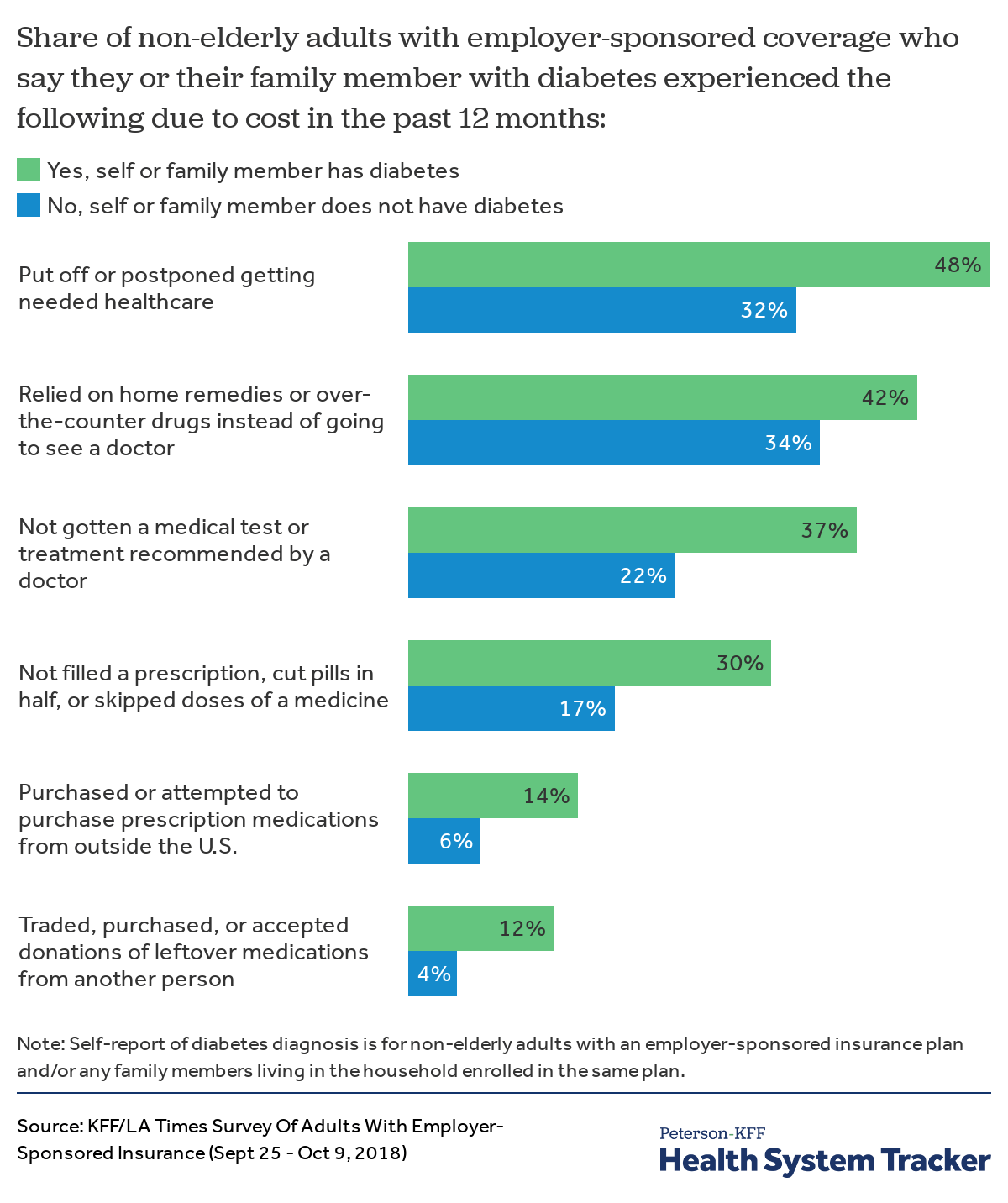
Among those with employer-sponsored health insurance, people with diabetes are more likely to postpone or delay treatment than those without diabetes
Among people with employer-sponsored insurance, those who either have diabetes or have a family member with diabetes covered by their health plan are more likely to postpone, delay, or skip treatment due to costs, compared to those without a diabetes diagnosis in the household. Those who either have diabetes themselves or have a family member with diabetes are also more likely to have used other tactics or alternatives to taking medication as prescribed because of the cost. For example, 30% of people with employer-sponsored coverage who have diabetes or have a family member with diabetes say they did not fill a prescription, cut pills in half, or skipped doses of a medicine because of the cost, compared to 17% of those without a diabetes diagnosis in the family. Additionally, in this coverage group, people with a diabetes diagnosis in the household are also more likely to rely on home remedies instead of going to the doctor, accept medications from other people, and purchase (or attempt to purchase) medications from outside the United States — all due to costs.
Among those with employer-sponsored health insurance, people with diabetes experience more difficulty affording healthcare than those without diabetes
Across the board, people with employer-sponsored insurance who either have diabetes or have a family member with diabetes covered by their plan are more likely to express difficulty affording monthly health insurance premiums and out-of-pocket cost-sharing, including medical bills that must be paid before meeting their deductible, co-pays for treatment as well as prescription drugs, and surprise medical bills. Overall, 58% of people with employer-sponsored coverage who either have diabetes themselves or have a family member with diabetes say they have had difficulty affording any type of healthcare or have any problems paying medical bills (including out-of-pocket payments), compared to 38% of those without a diabetes diagnosis in the household.
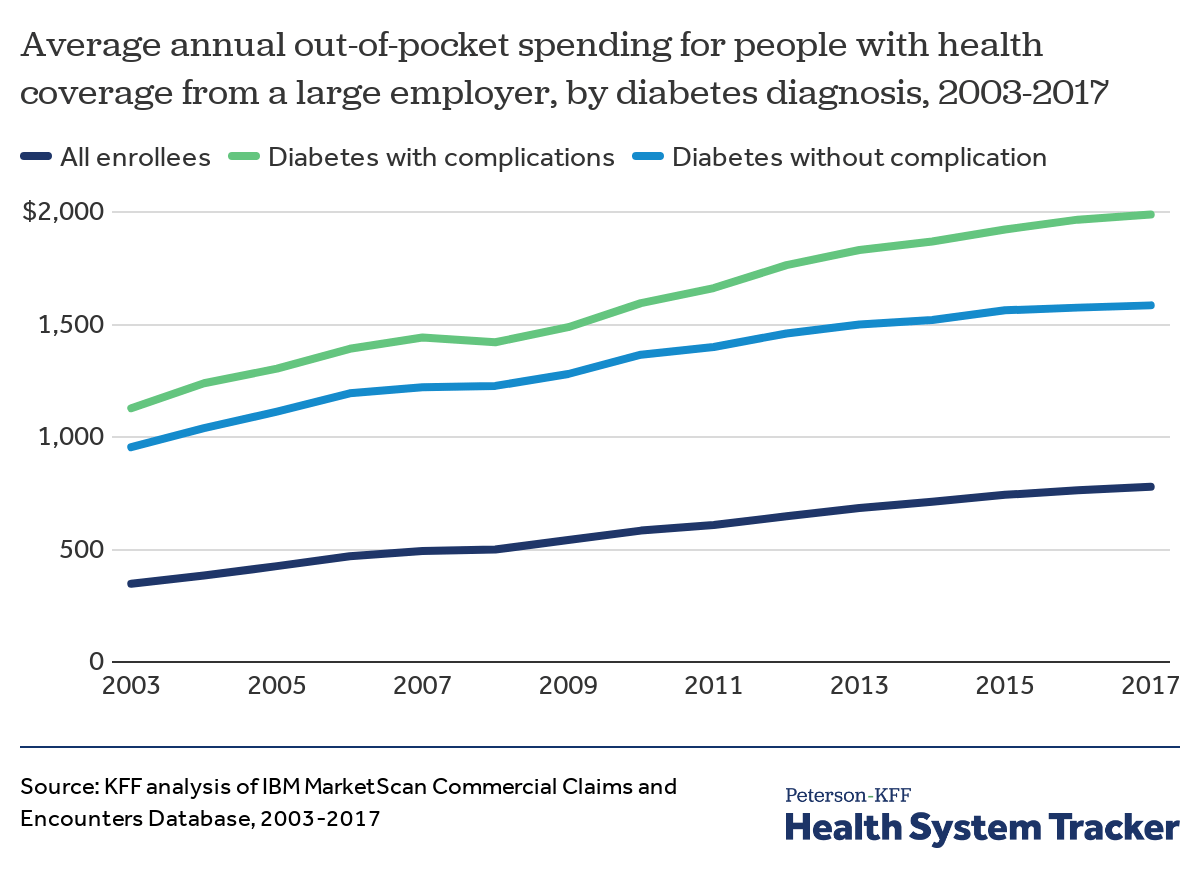
People with diabetes with large employer coverage have twice the average out-of-pocket spending compared to all enrollees
People enrolled in large employer coverage who have diabetes face annual out-of-pockets costs more than double that of all enrollees with large employer coverage. Average annual out-of-pocket spending for all enrollees increased by approximately 124% from 2003 to 2017 (from $348 to $779). Meanwhile, among enrollees with a diabetes diagnosis, average annual out-of-pocket spending increased by 76% (from $1,128 to $1,989) for those with diabetes complications and by 66% (from $955 to $1,585) for those without complications.
Health Spending
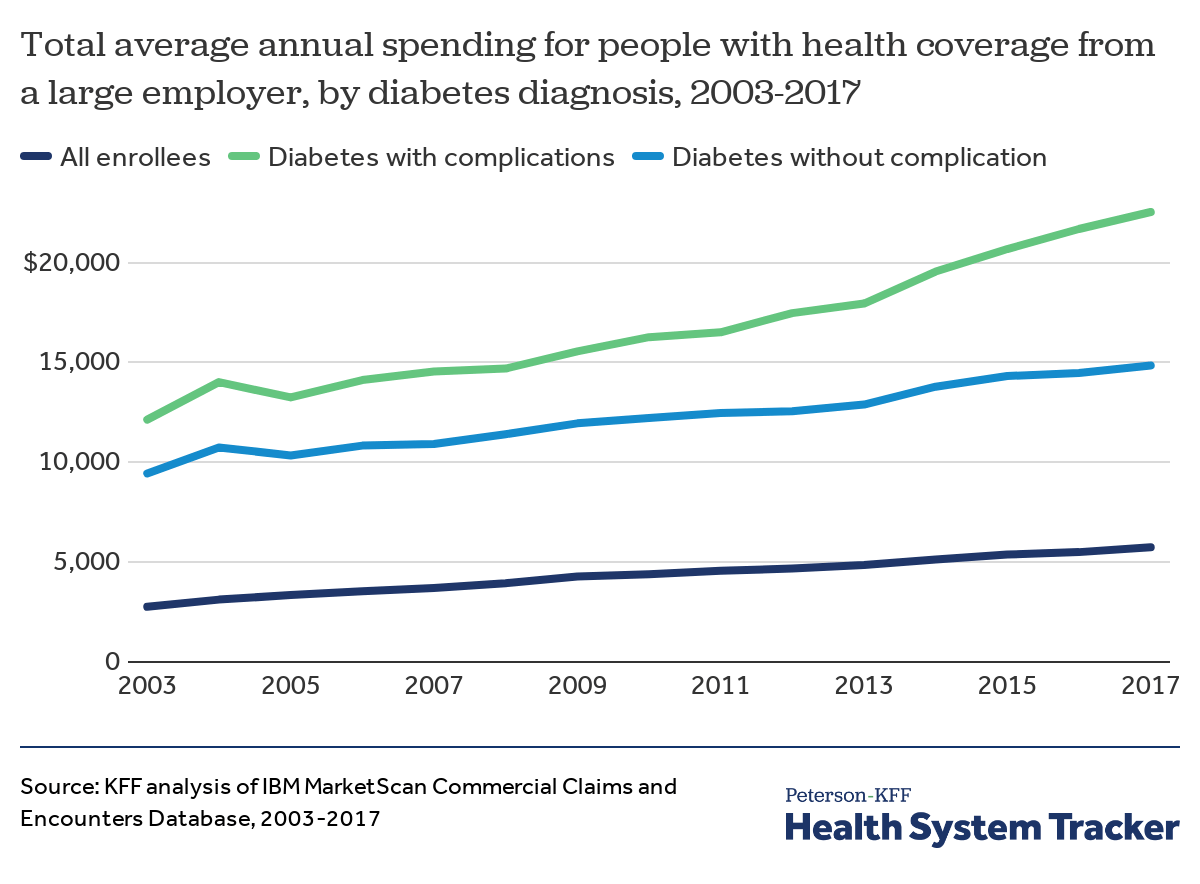
Among people with large employer coverage, spending on healthcare is much higher for enrollees with diabetes than for all enrollees
Compared to average annual spending for all enrollees with large employer coverage, spending is much higher for enrollees with a diabetes diagnosis. Average annual health spending for all enrollees grew by 108% from 2003 to 2017 (from $2,767 to $5,747). In that time, average annual spending increased 86% (from $12,137 to $22,532) for enrollees diagnosed with diabetes with health complications and 57% (from $9,443 to $14,850) for those diagnosed with diabetes without a health complication.
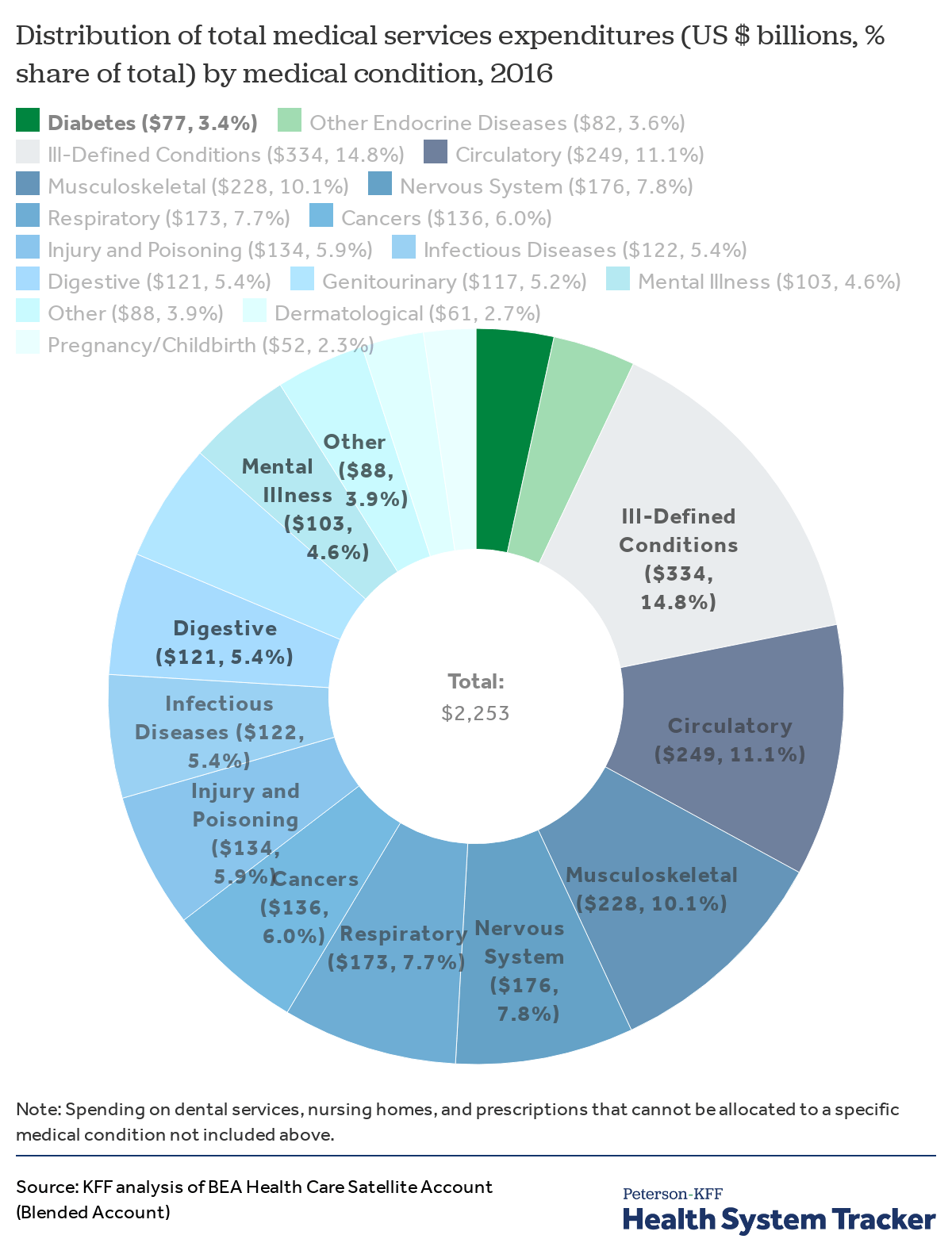
Spending on endocrine diseases accounts for seven percent of medical condition-based health expenditures
In 2016, the U.S. spent approximately $77 billion on the treatment of diabetes, according to estimates by the Bureau of Economic Analysis. This represents 3.4% of total medical services spending on treatment of diseases and other medical conditions ($2.25 trillion).
In 2016, diabetes and other endocrine diseases together accounted for 7% of total spending on medical conditions, at $159 billion. The top 6 medical condition-based spending categories (ill-defined conditions, and diseases of the circulatory system, musculoskeletal system, nervous system, respiratory system, and endocrine system) account for over half (59%) of all medical services spending by medical condition.
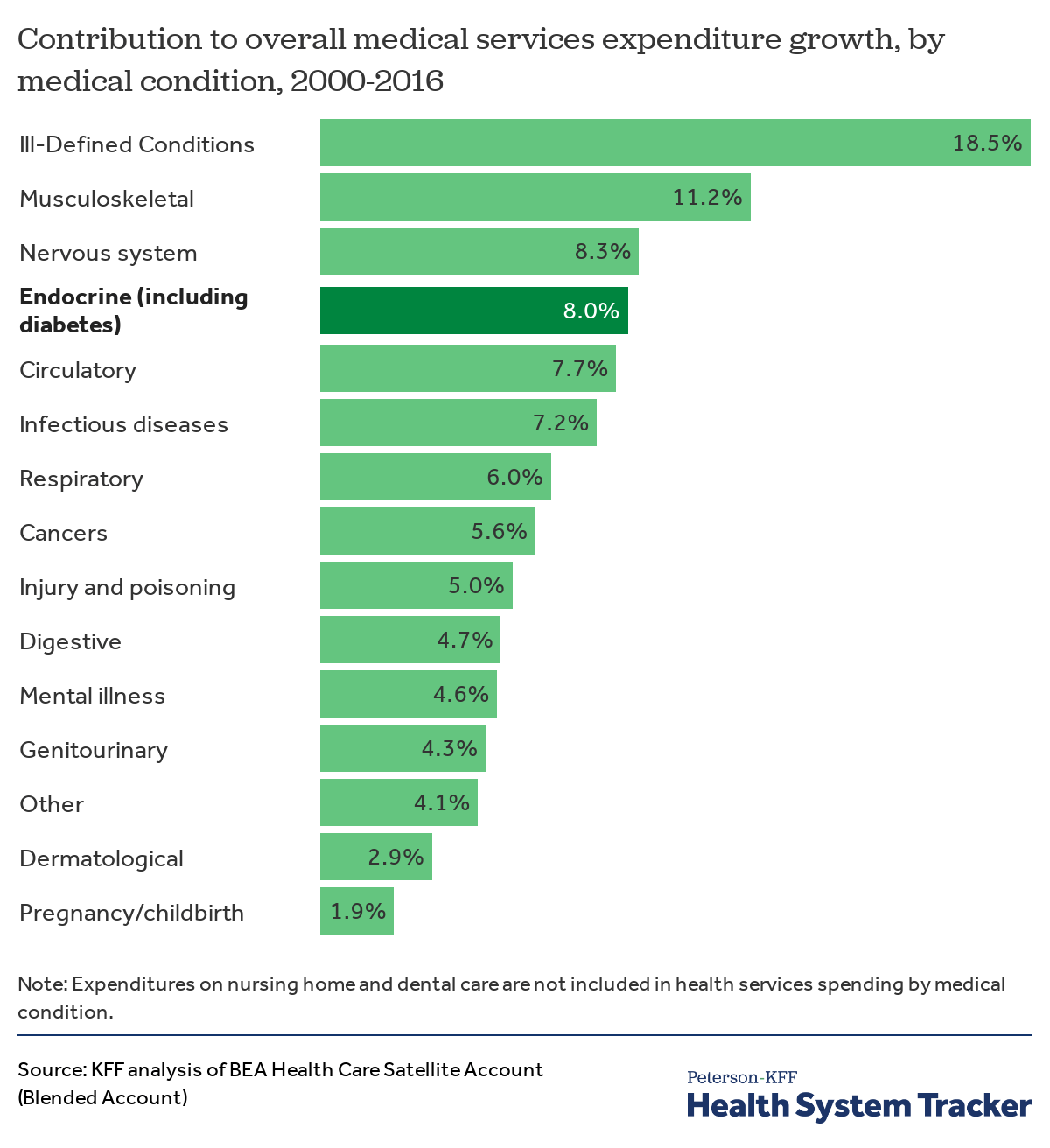
Diabetes and other endocrine diseases are a leading driver of medical services spending growth
Endocrine, nutritional, and metabolic diseases and immunity disorders – including diabetes – accounted for 8% of medical services spending growth from 2000 to 2016. Diabetes alone accounted for 4.2% of total medical services expenditure growth. Overall, medical services expenditures grew by 66.6% between 2000 and 2016. Total spending in this chart factors in changes in prevalence of a medical condition as well as the price of medical services.
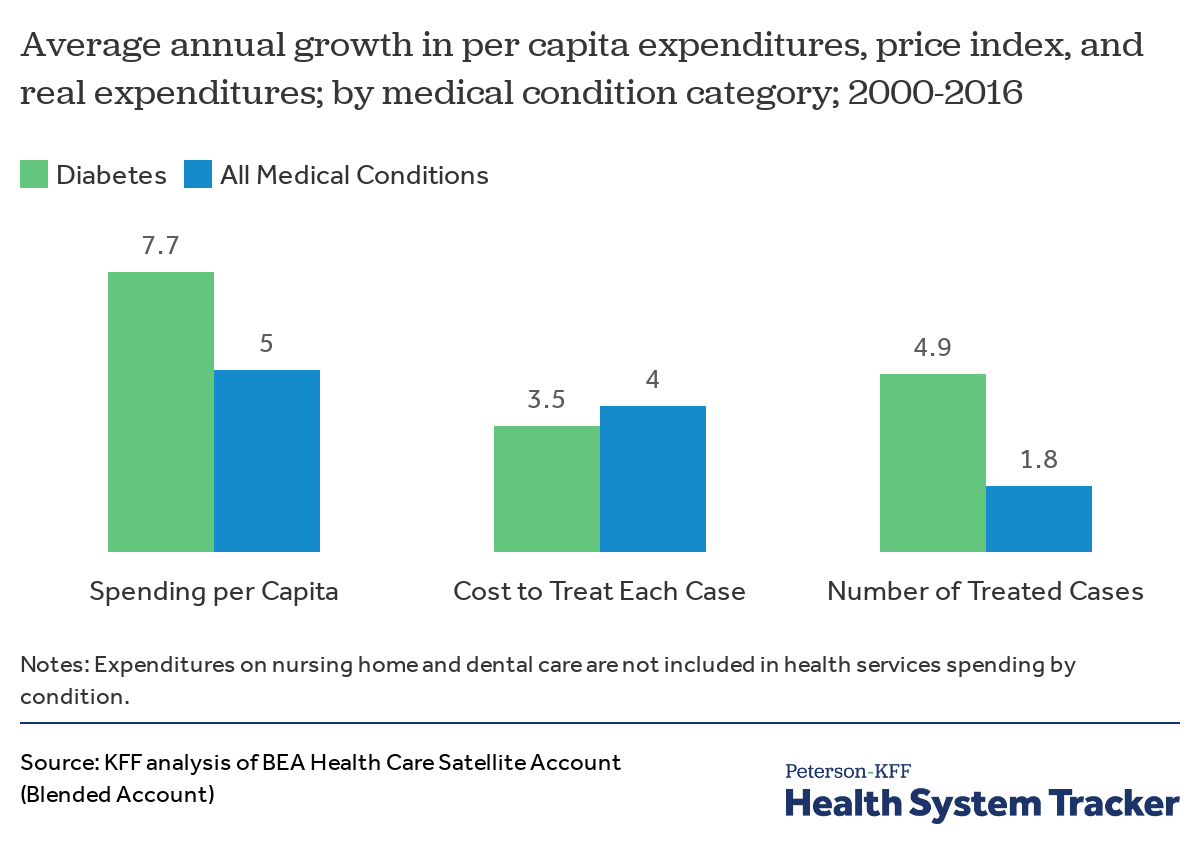
Average growth in per capita spending for endocrine diseases was higher than the average for all medical condition-based categories
Between 2000 and 2016, the average annual growth in per capita expenditures for diabetes was higher than the average growth in spending on all medical condition categories. In this analysis, spending is calculated for a particular medical condition or disease, rather than by service. Growth in spending on diabetes care over the period was driven by both increases in the number of people being treated for these conditions and increases in the costs of treatment.
The annual cost to treat a case of diabetes rose 74% from 2000 to 2016 ($1,209 to $2,106). Per capita spending on diabetes increased 228% from 2000 to 2016 ($72 to $238). Overall, U.S. spending on treatments for endocrine diseases and other related nutritional and metabolic conditions increased 177% from 2000 to 2016 (from $177 to $491 per capita). During this time, U.S. spending on all medical conditions increased 118% between 2000 and 2016 (from $3,192 to $6,974 per capita).
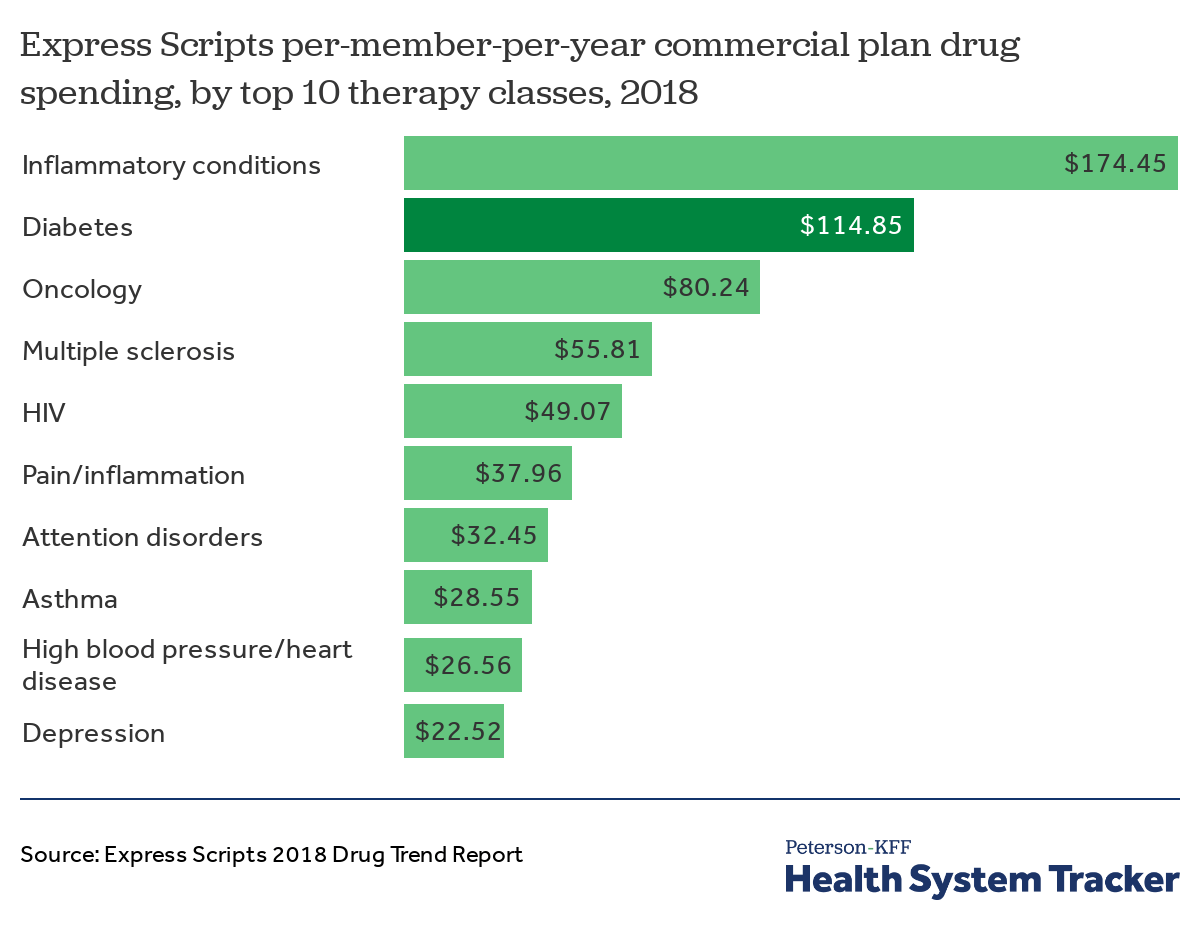
Diabetes medications were the second most costly therapy class drugs in 2018
The Express Scripts 2018 Drug Trend Report finds that medications for diabetes were the second most costly therapy class drugs in 2018, ranked based on per-member-per-year (PMPY) spending. Spending on diabetes medications was $115 PMPY in 2018, second only to $174 PMPY spending on medications for inflammatory conditions (e.g., rheumatoid arthritis, psoriasis). While PMPY spending for most of the top five therapy classes is driven primarily by spending on specialty drugs, diabetes is the exception, with spending only on traditional drugs.
Health Status and Outcomes
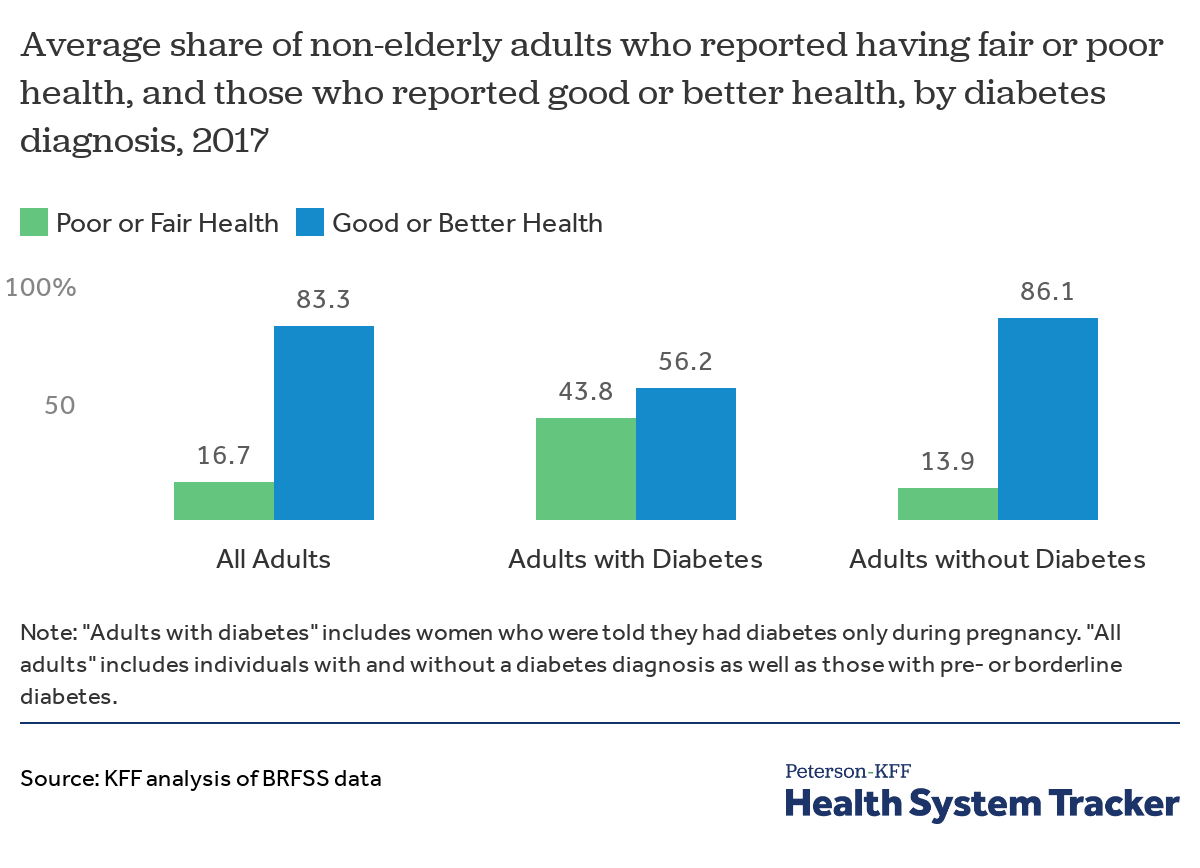
Four in ten adults with diagnosed diabetes report poor or fair health
About 4 in 10 (43.8%) adults with a diabetes diagnosis report that their health is fair or poor, compared to over 1 in 10 (13.9%) of adults without a diabetes diagnosis. While most (83.3%) adults report being in good or better health, that share is much lower for adults with a diabetes diagnosis (56.2%).
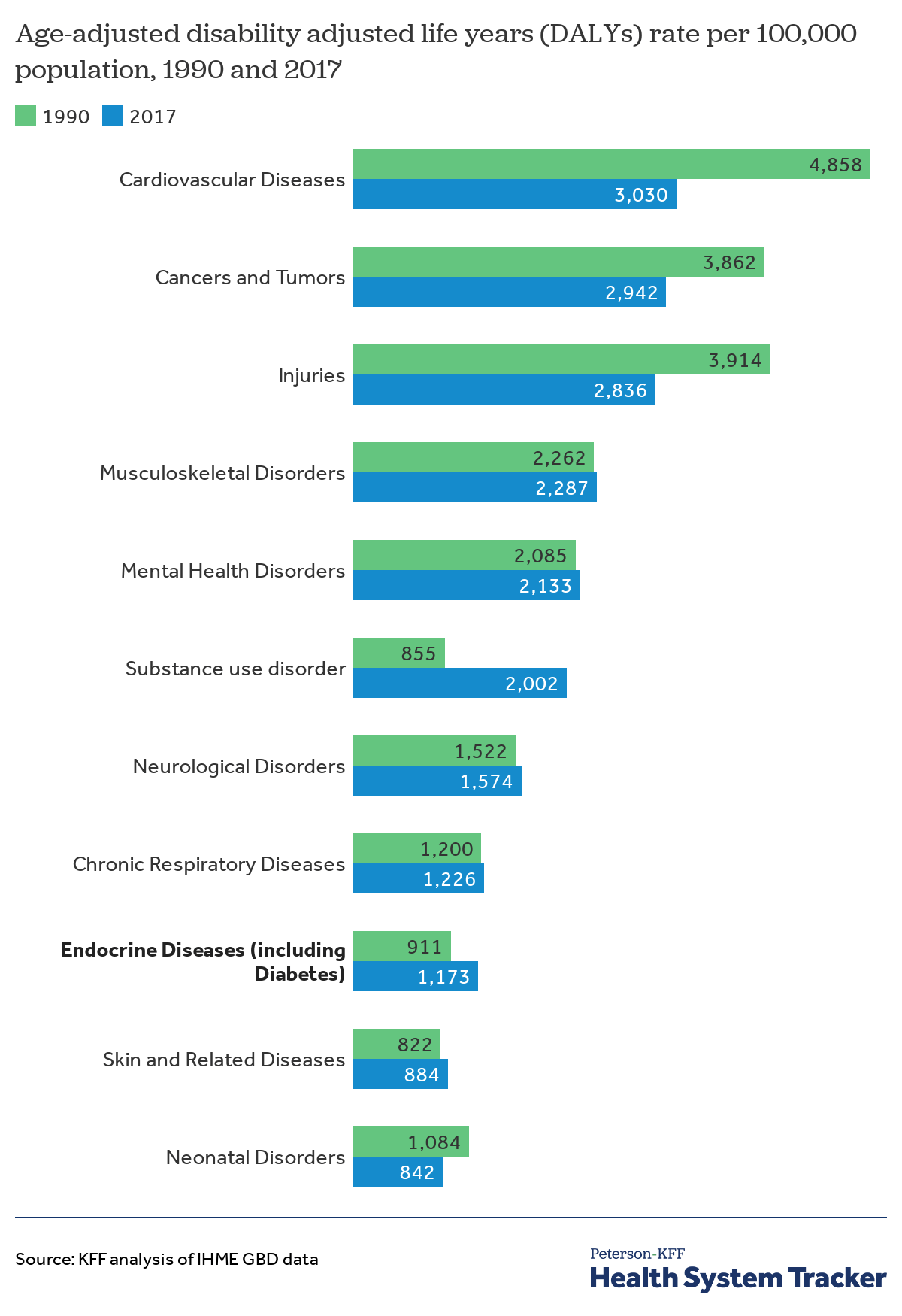
U.S. disease burden for endocrine diseases has increased over the past three decades
Aside from mortality and diagnosis rates, another way to measure the effect diabetes has on health is to look at the burden of disease, which takes into account both years of life lost due to premature death as well as years of productive life lost to poor health or disability. Using a measure called Disability Adjusted Life Years (DALYs), the Institute for Health Metrics and Evaluation finds that diabetes and kidney diseases were the ninth leading cause of disease burden in the U.S. in 2017. For the diabetes and kidney disease category, the growth in age-standardized DALYs stems from increases in both years of life lost and years lived with disability.
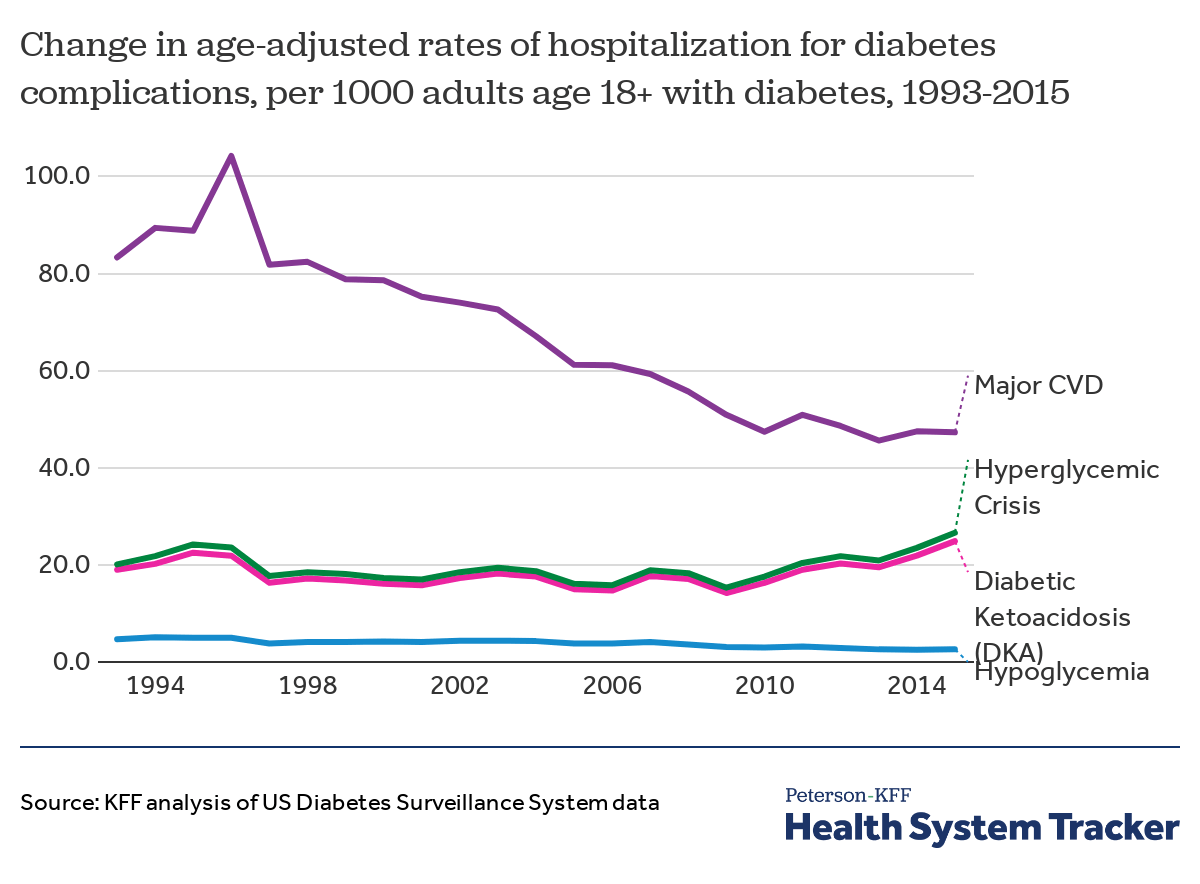
Hospitalization rates for some diabetes complications have declined over time
Between 1993 and 2015, the rate of hospitalizations among adults with diabetes rose by 32% for those hospitalized due to hyperglycemic crisis (from 20.1 to 26.6 hospitalizations per 1,000 adults) and 31% for diabetic ketoacidosis (from 19 to 24.9 hospitalizations per 1,000 adults). Meanwhile, the hospitalization rate improved by 45% for hypoglycemia (from 4.7 to 2.6 hospitalizations per 1,000 adults) and by 43% for major cardiovascular disease (from 83.3 to 47.3 hospitalizations per 1,000 adults).
Hospitalizations for diabetes complications differ by age. Diabetic ketoacidosis is an acute, life-threatening condition caused by high blood sugar levels that persist for too long, leading to a build-up of acids in blood. Hyperglycemic crisis is caused by chronically high blood glucose levels and can lead to complications such as, stroke, heart attack, amputation, and kidney disease. Both complications occur most often for patients with type 1 diabetes, who also tend to be younger — thus, adults with diabetes between the ages 18-44 experience most hospitalizations for both diabetic ketoacidosis and hyperglycemic crisis. Meanwhile, those ages 75 and up are most likely to be hospitalized for hypoglycemia (very low blood sugar) or major cardiovascular disease. Preventive health care and management of risk factors are among the primary reasons for a decline in severe diabetes complications.
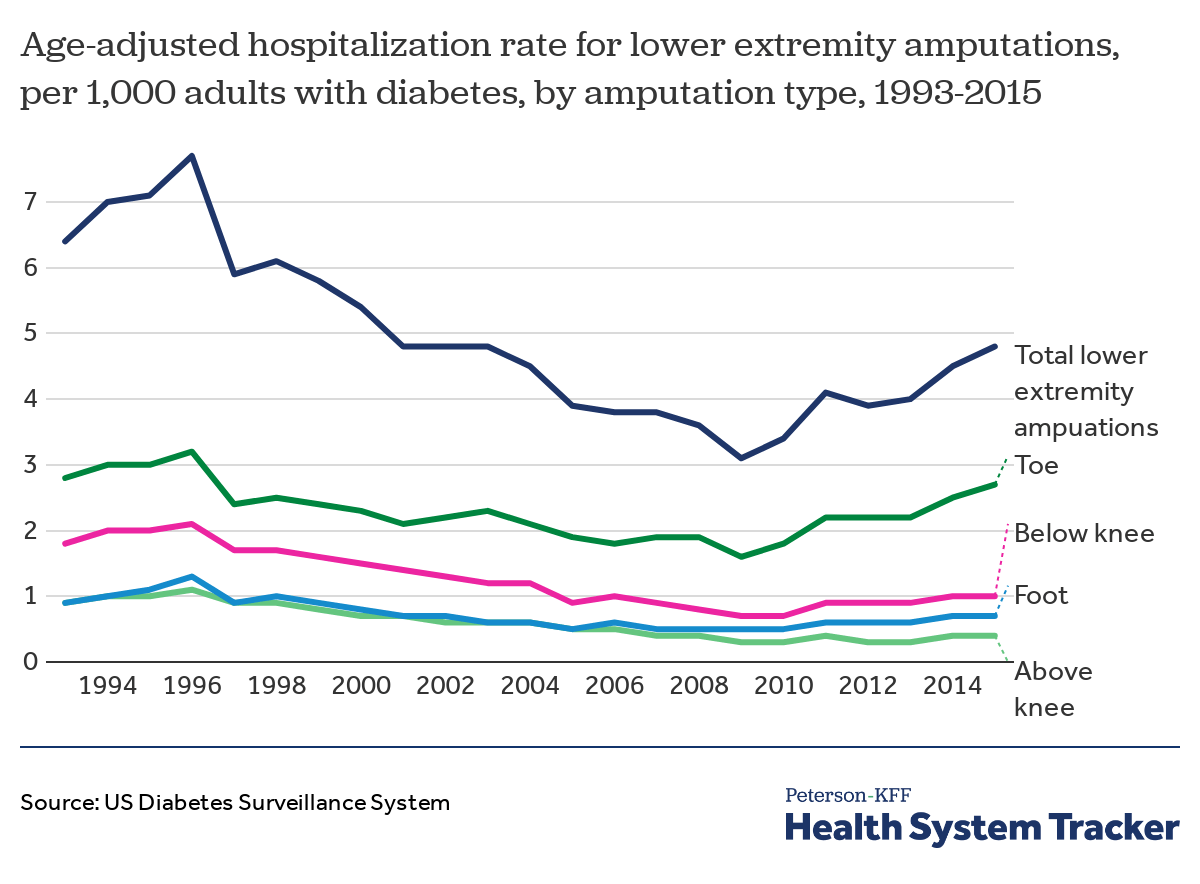
Diabetes patients have been increasingly hospitalized for lower extremity amputations since 2009
Diabetes complications such as nerve damage and poor blood circulation can put patients at risk of lower limb amputation. Most diabetes-related lower extremity amputations result from foot sores, which can often be prevented with diabetes management and foot care. Although the rate of hospitalizations for such amputations has dropped over time, diabetes patients have increasingly been hospitalized for lower limb removal in recent years. According to the CDC, between 2009 and 2015, the rate of hospitalizations for lower extremity amputations among adults with diabetes increased 55% (from 3.1 to 4.8 hospitalizations per 1,000). In that time, hospitalizations specifically for toe amputations among diabetes patients increased 69% (from 1.6 to 2.7 hospitalizations per 1,000).