On June 21, 2024, the 5th Circuit Court of Appeals affirmed the district court’s ruling that the ACA’s requirement to cover without cost-sharing services recommended by United States Preventive Services Task Force (USPSTF) is unconstitutional. However, the 5th Circuit ruled that a nationwide remedy was not proper and that only the plaintiffs are permitted to exclude USPSTF recommended services from their plans. The Appeals Court sent back to the district court the plaintiffs’ claim that the Secretary of Health and Human Services’ ratification of HRSA and ACIP recommendations violates the Administrative Procedure Act for further briefing and a judgment.
The Affordable Care Act (ACA) requires most private health plans to cover in-network preventive services at $0 cost-sharing for enrollees. This preventive services coverage mandate was ruled partially unconstitutional by the U.S. District Court in the Northern District of Texas in Braidwood Management v. Becerra. On March 30, 2023, the Texas district court excluded from the requirement all preventive care recommendations issued by the United States Preventive Services Task Force (USPSTF) on or after March 23, 2010, when the ACA was signed into law. (For examples of preventive care services that may be affected by the Braidwood district court ruling, see here.)
The Biden administration is appealing this decision. On May 15, 2023, the Fifth Circuit Court of Appeals issued an administrative stay, putting a temporary pause on the effect of the Texas district court ruling. Separately, and prior to the stay, major private health insurers announced that they do not plan to make changes to coverage of preventive services until a final ruling has been made. Some insurers and employers may introduce cost sharing over time if the district court ruling holds.
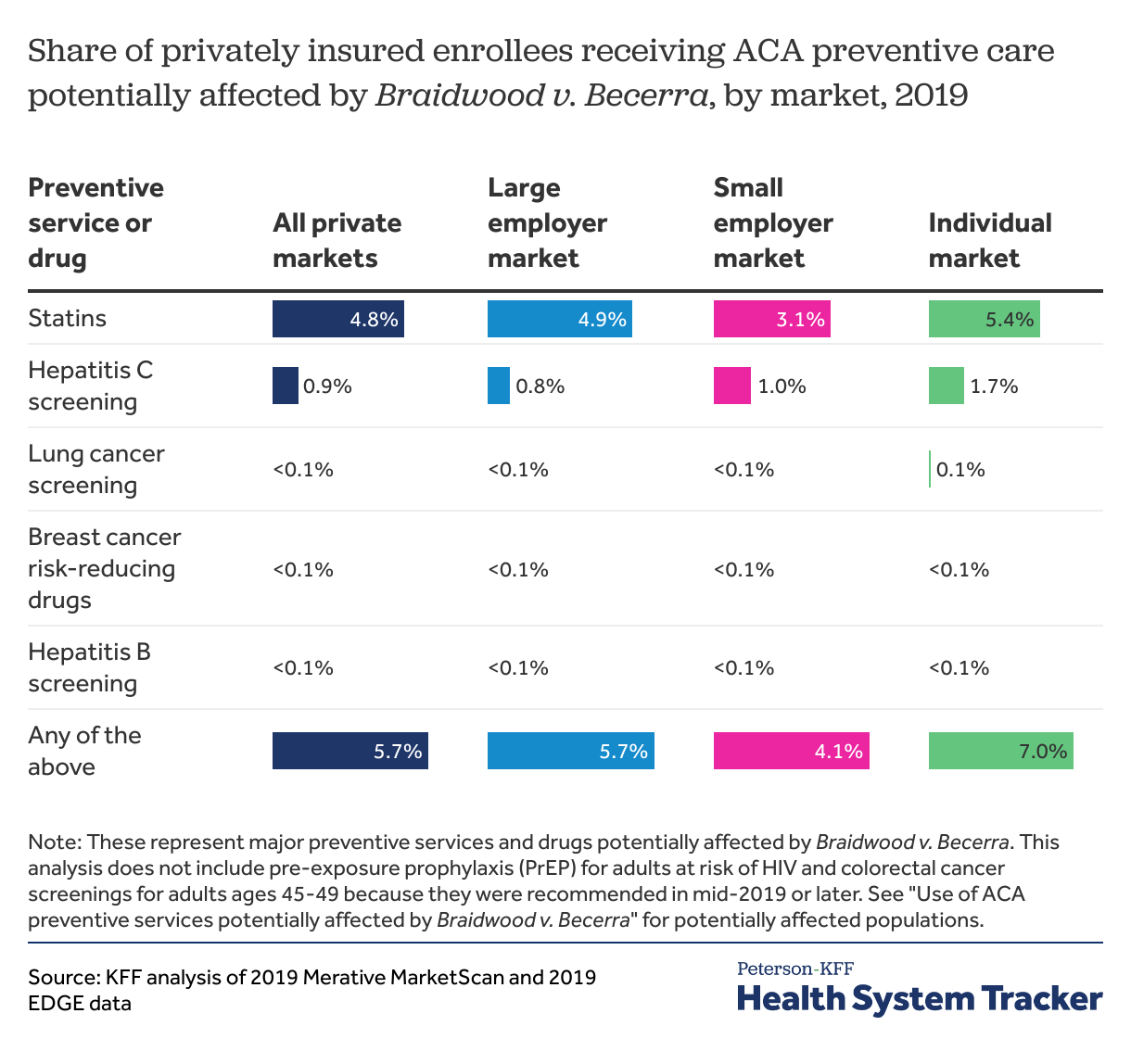
In this analysis, we find that at least 1 in 20 privately insured people (5.7%) received any of the ACA preventive services or drugs potentially affected by Braidwood Texas district court ruling. According to the American Community Survey, 173 million non-elderly people have private health insurance coverage. Based on this, we estimate up to nearly 10 million people could face higher out-of-pocket costs if the district court ruling stands and insurers ultimately decide to implement cost-sharing.
In 2019, about 10 million people used preventive care potentially affected by Braidwood
We use similar methods for analyzing preventive care utilization as those outlined in a KFF/RTI brief published before the district court’s ruling. In this analysis, we use 2019 claims data to reflect utilization in a typical pre-pandemic year. We use this older data because preventive services utilization changed significantly during the COVID-19 pandemic. We focus on most of the preventive services and drugs with major changes to USPSTF recommendations after 2010, though other services may also be affected by the district court ruling. This analysis specifically includes:
- statins for adults ages 40 to 75 who are at risk for cardiovascular disease,
- hepatitis C screening for adults ages 22 and older,
- lung cancer screening for all adults,
- breast cancer risk-reducing drugs for at-risk women ages 35 and older, and
- hepatitis B screening for non-pregnant, at-risk adults ages 22 and older.
Since we are using 2019 data, our analysis does not include more recent USPSTF recommendations, including pre-exposure prophylaxis (PrEP) for adults at risk for HIV (recommended in June 2019) and colorectal cancer screenings for average-risk adults ages 45 through 49 (recommended in May 2021).
In 2019, 7.0% of people enrolled in the individual market (those purchasing health coverage directly through ACA exchanges or health plan websites) received preventive care affected by Braidwood district court decision. Slightly smaller shares of people who are insured through a large employer (5.7%) or a small employer (4.1%) received these preventive services and drugs. Statins were the most commonly used form of ACA preventive care potentially affected by Braidwood district court ruling.
Discussion
While the Fifth Circuit Court’s stay is in effect, the federal government can continue to enforce the ACA preventive services mandate for everyone except the plaintiffs in the case. If the Fifth Circuit Court stay is lifted and the district court’s decision is affirmed by a higher court, insurers would be allowed to introduce cost-sharing for any of the affected preventive services and drugs or exclude coverage altogether, though the latter appears to be the less likely scenario.
Though we estimate about 10 million people received any of these forms of preventive care at $0 cost-sharing in 2019, we do not include colorectal cancer screenings for adults in their late 40s or PrEP, which were recommended on or after 2019. As a result, the number of people who could be affected by cost-sharing or coverage loss for these services may be higher than this analysis shows. While the total number of people on PrEP is relatively small (366,458 in 2021), the majority (an estimated 81%) have private health coverage and are potentially impacted by this case. The cost of PrEP drugs, labs, and provider visits can be high. Similarly, colonoscopies can be quite expensive, averaging over $1,000.
Additionally, the ruling could affect more services and people over time – as new preventive services and drugs are developed, recommended, and adopted. If the higher courts fully side with the plaintiffs, the effects could be more sweeping and open the door for future employer objections to other preventive services coverage at $0 cost share. Our earlier analysis with RTI international found 6 in 10 privately insured people, or about 100 million people, received services covered under the ACA preventive services mandate in a typical year and discusses further implications of this case.
Krutika Amin, Shameek Rakshit, Cynthia Cox, and Gary Claxton are with KFF. Allison Carley is with RTI International.
Acknowledgement: The authors would like to thank with RTI International for their contribution to an earlier analysis, on which this analysis draws.
The Peterson Center on Healthcare and KFF are partnering to monitor how well the U.S. healthcare system is performing in terms of quality and cost.