In December 2020, Congress passed the “No Surprises Act,” which prohibits most surprise out-of-network billing for plan years beginning in 2022. Surprise bills occur when a patient receives care from an out-of-network provider or facility during an emergency visit or while receiving non-emergency care at an in-network hospital or facility. In these cases, patients may face balance billing from the out-of-network provider for the difference between the provider’s charged amount and the plan’s allowed amount for that service. Additionally, patients may have higher plan cost sharing for out-of-network services. We have previously found that among large group health plan enrollees, 1 in 5 emergency room visits and 1 in 6 in-network hospital admissions potentially led to a surprise medical bill.
The No Surprises Act requires plans to apply in-network cost sharing and prohibits out-of-network providers from balance billing on surprise medical bills. Additional details on the No Surprises Act are available here. The law’s protections, however, do not apply to bills for ground ambulances, which Congress put off pending further study. The No Surprises Act requires the Departments of Labor, Health and Human Services, and Treasury to appoint an advisory committee that will review and recommend options to protect patients from ground ambulance surprise bills.
This brief describes ambulance use, ownership type, the share of ground ambulance rides with a potential for surprise bills, and state or local policies aimed at reducing surprise bills for ground ambulances. Key findings include:
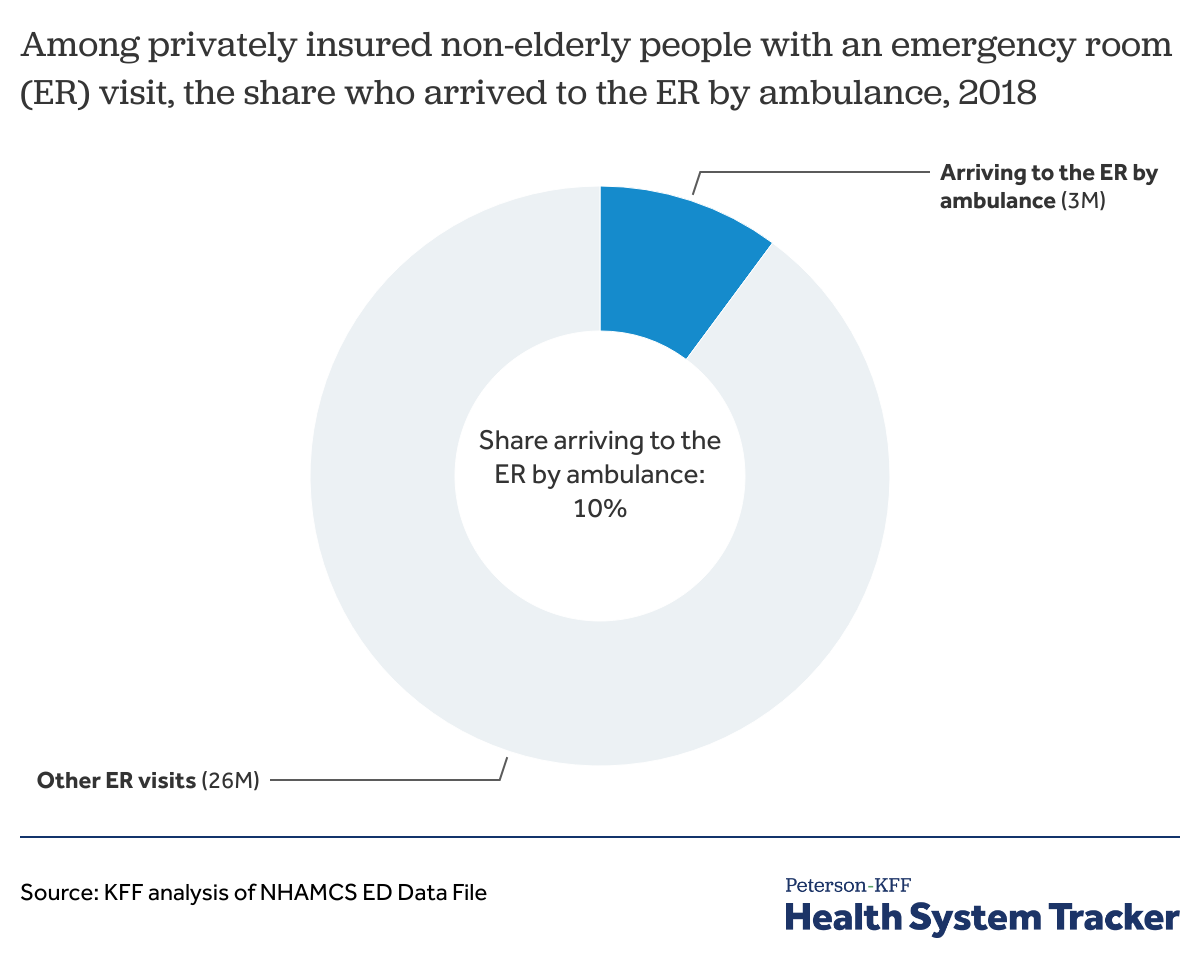
- Ambulances bring 3 million privately insured people to an emergency room each year.
- Local fire departments and other government agencies provide nearly two-thirds (62%) of emergency ground ambulance rides.
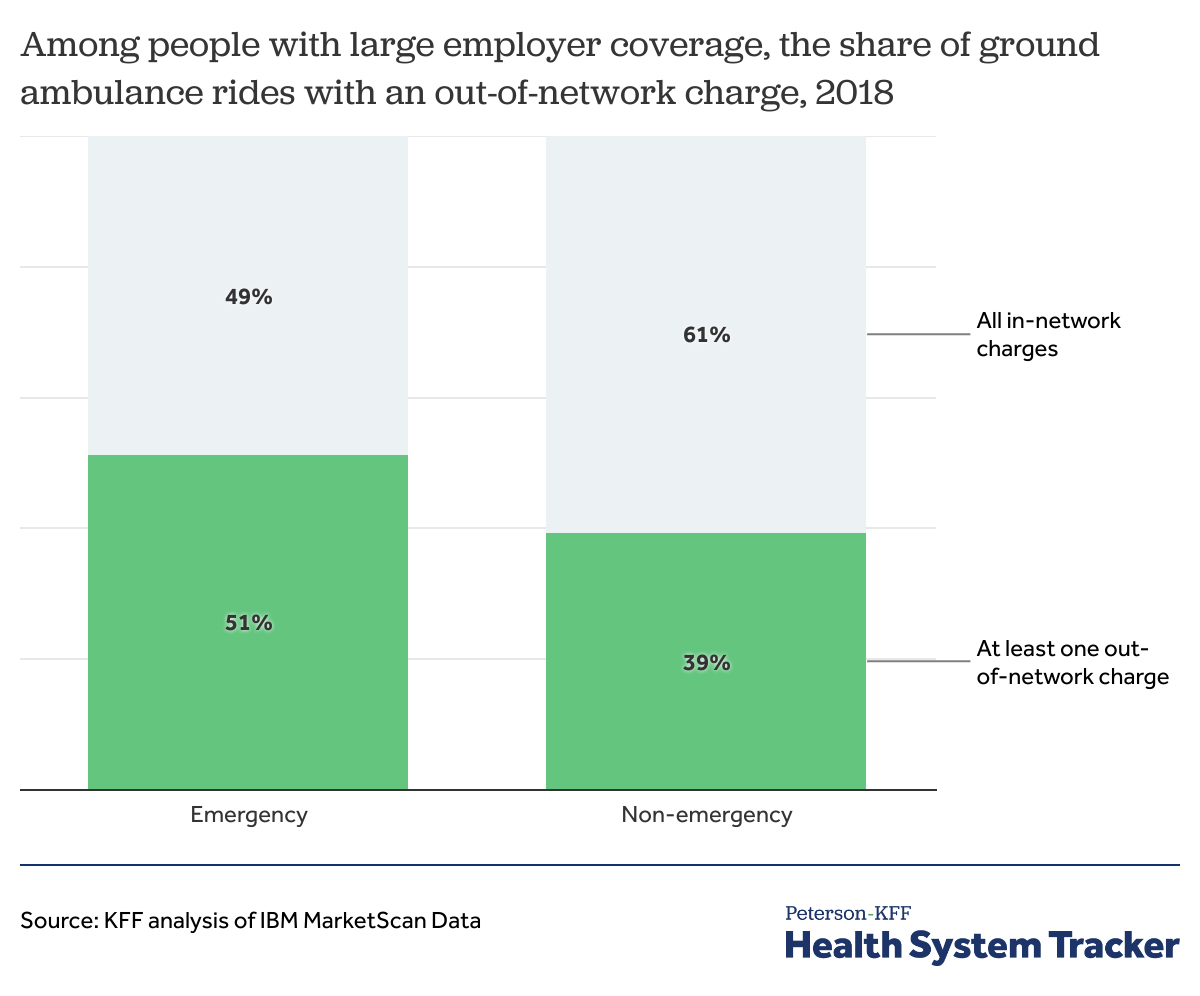
- About half (51%) of emergency and 39% of non-emergency ground ambulance rides included an out-of-network charge for ambulance-related services that may put privately insured patients at risk of getting a surprise bill.
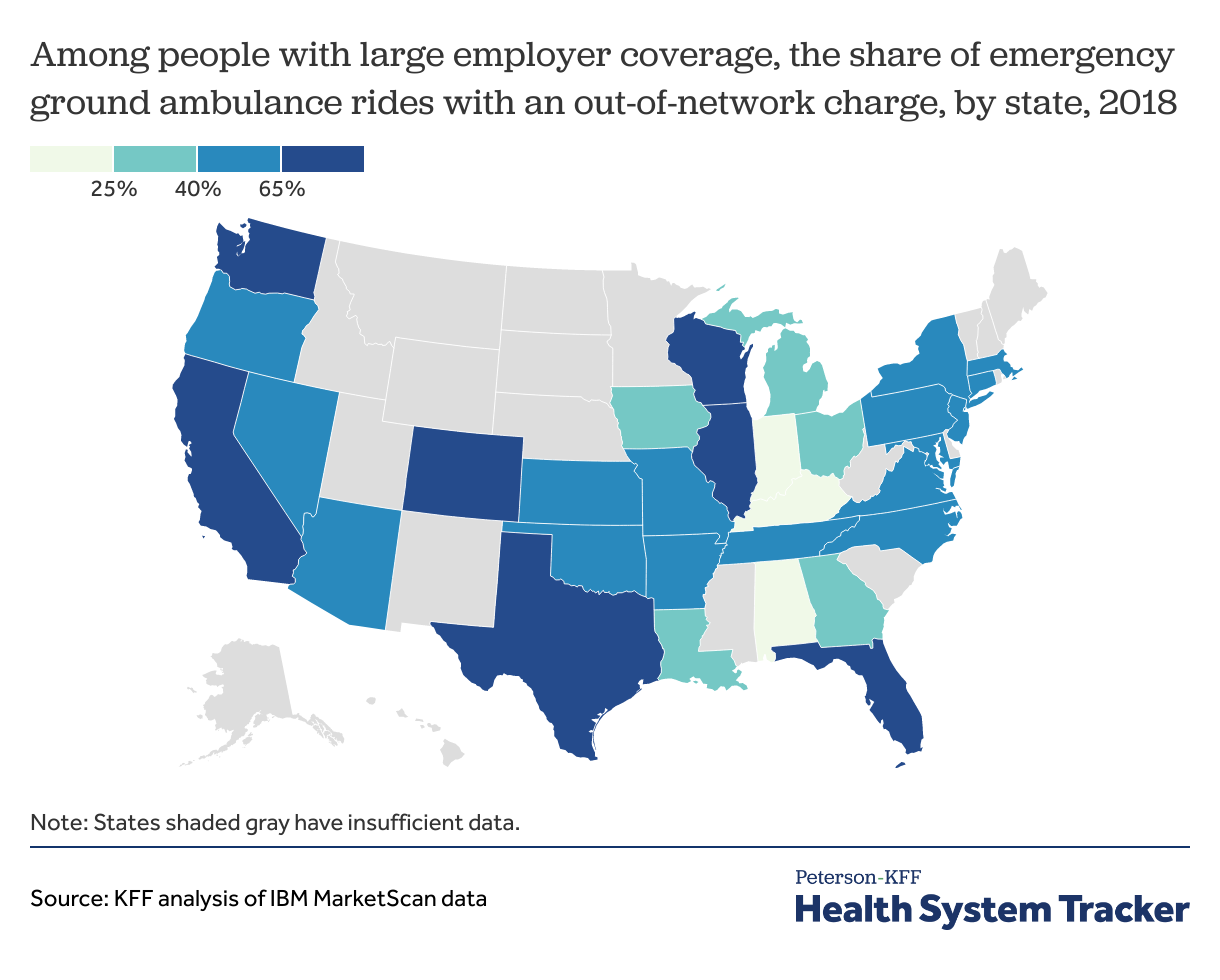
- In seven states (Washington, California, Florida, Colorado, Texas, Illinois, and Wisconsin), over two-thirds of emergency ambulance rides included an out-of-network charge for ambulance-related services that may pose a surprise bill risk.
Frequency of ground ambulance rides
Ambulances bring about 3 million people with private health insurance to the emergency room each year
Using data from the National Hospital Ambulatory Medical Care Survey (NHAMCS), we estimate that there were 29 million emergency room visits by privately insured patients in 2018. About 10% of these emergency room patients (3 million people) were brought to the emergency room by an ambulance.
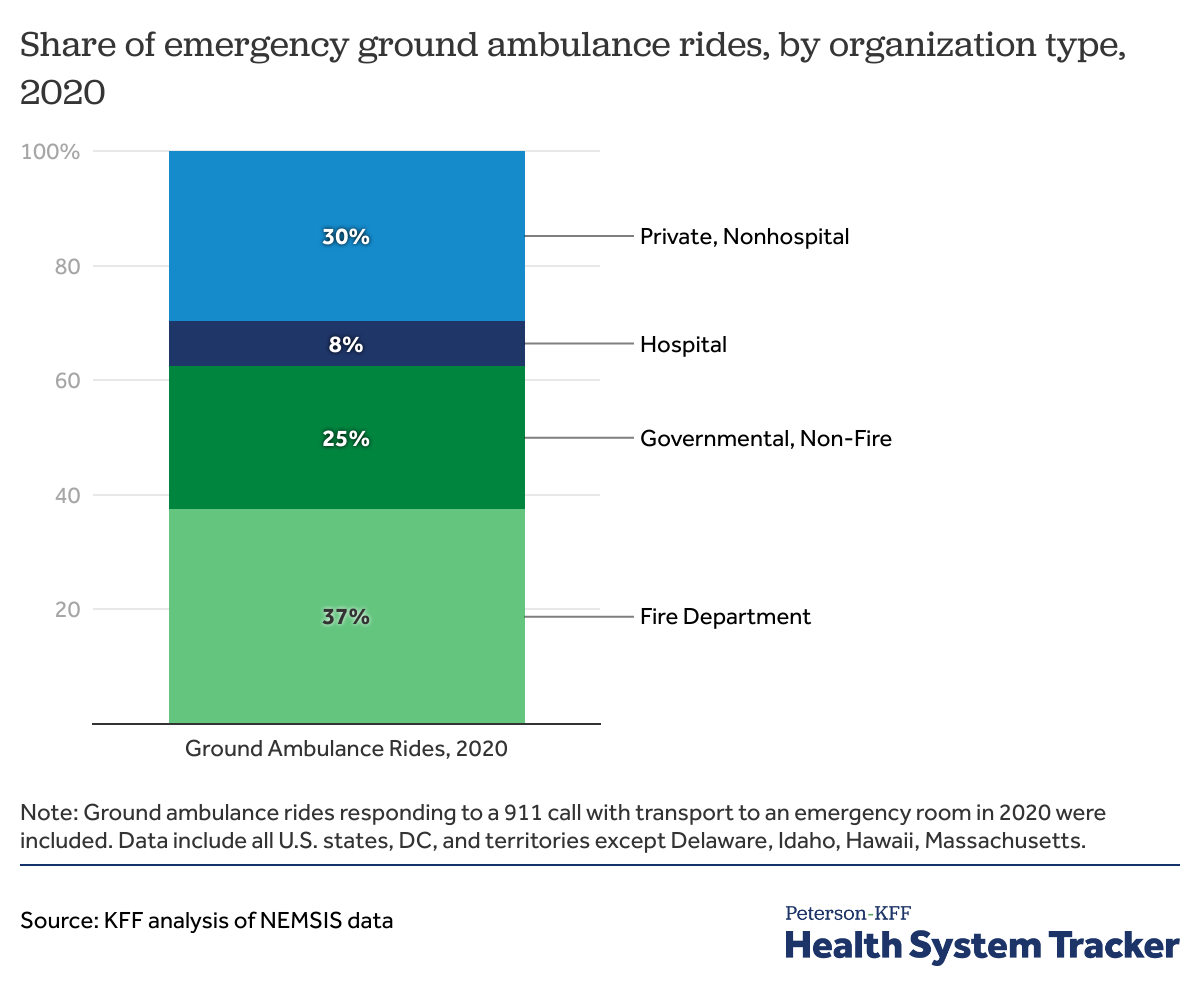
Almost 2 in 3 emergency ground ambulance rides were provided by government-based organizations in 2020
Many emergency medical transport services are operated by municipal and county governments, and therefore, may be subject to additional types of state and local regulation. Some municipal ground ambulance services may not contract with private insurance companies. Some publicly-operated ground ambulances may provide services as a public benefit and prohibit patient billing, as we discuss further below. State and local regulation and operation of ground ambulances was reportedly one reason that Congress did not include ground ambulances in the No Surprises Act.
Read more from
Surprise BIlls
See more briefs and data.
Using the National Emergency Medical Services Information System (NEMSIS) data, we find that 62% of emergency ground ambulance rides were provided by fire departments (37%) or other government (25%) organizations in 2020. Additionally, 30% of emergency ground ambulance rides were provided by private non-hospital ambulance companies and another 8% were provided by ambulances owned by hospitals.
Risk of surprise billing for ground ambulance rides
About half of emergency ground ambulance rides among privately insured people pose a risk of a surprise bill
Using 2018 large employer claims data we find that 51% of emergency ground ambulance rides and 39% of non-emergency ground ambulance rides included an out-of-network charge for ambulance-related services, putting the patient at risk of a surprise medical bill.
For many of the largest states, at least two-thirds of ground ambulance rides pose a risk of surprise bills
In seven states (Washington, California, Florida, Colorado, Texas, Illinois, and Wisconsin), more than two-thirds of emergency ground ambulance rides had an out-of-network charge for ambulance-related services. In Alabama, Kentucky, and Indiana, fewer than 25% of emergency ground ambulance rides included an out-of-network charge.
The roles of federal, state, and local governments in regulating ground ambulance billing
In the absence of federal laws protecting patients from ground ambulance surprise bills, states and local governments play varying roles in regulating ground ambulance patient billing and insurer payments. There are two types of state laws that are important here: laws that regulate ambulance providers and laws that regulate how insurers treat claims from ambulance providers. While states cannot regulate the self-funded health plans that cover about two-thirds of workers in the U.S. (typically those employed at larger companies), state governments do regulate health insurers selling fully-insured coverage. Many states specifically protect patients from getting a ground ambulance surprise bill from providers. However, some of these state regulations only apply to a subset of ground ambulance agencies.
State and local laws vary in whether ground ambulance service providers or health plans are regulated and types of ground ambulances that are prohibited from balance billing patients. For example,
- Baltimore County operated emergency medical services do not bill county residents for ambulance services. Under this county benefit, county-funded emergency medical services can bill the patient’s insurance (private insurance, Medicare, or Medicaid) to recoup the costs. Non-county residents who use Baltimore County ambulances can be billed the entire cost.
- Colorado state law requires state-regulated health plans to reimburse out-of-network private ground ambulances at 325% of Medicare payment rates and limits the amount patients pay out-of-pocket to the in-network rate. Under this Colorado state law private ambulance services are prohibited from billing insured patients other than for the in-network cost sharing rate (deductible, coinsurance, or copayment). Though, this Colorado state law does not apply to publicly-funded fire departments.
- Connecticut requires ambulance providers to make good faith effort to first charge the patient’s health insurer, but if the health insurer does not pay or declines the claim, then the ambulance provider can bill the patient.
- Delaware has regulations on out-of-network payment dispute resolution process for health plans and providers of emergency services, which specifically include ground ambulances.
- Iowa protects patients from getting surprise bills for emergency services, but ground ambulances are not explicitly mentioned in Iowa’s regulations.
- Maryland prohibits local government, volunteer, or fire department owned ground ambulances from billing patients. Other ambulances in Maryland may bill patients directly to recoup some or all costs.
- New York prohibits ground ambulance service providers from billing enrollees in certain plan types (HMOs, PPOs, EPOs) more than the in-network cost sharing.
- Texas state law protects patients enrolled in state-regulated plans from surprise bills in certain situations. Texas state regulators interpreted the law to include ground and air ambulances. However, a lawsuit deemed application of the state regulations to ground and air ambulances to exceed the state’s authority, and therefore, patients are not protected from receiving surprise bills for ground ambulances in Texas.
Protecting patients from surprise bills for ground ambulances requires additional considerations. The services that government-owned ground ambulances provide as a public benefit may be different than those that private ground ambulances provide. Billing practices may also differ for government-based or private ground ambulances.
Discussion
The No Surprises Act will prohibit most surprise bills, reducing out-of-pocket costs for emergency services and non-emergency services where the patient unintentionally sees an out-of-network provider. Congress did not include ground ambulances in the No Surprises Act reportedly because so many emergency medical transport services are operated by municipal and county governments, and therefore, may be subject to additional types of state and local regulation. Congress expressed interest in revisiting surprise billing for ground ambulances once it gathers more information.
One-in-ten emergency room visits for privately insured patients begin with an ambulance ride. Similar to other studies, we find that about half of emergency ground ambulance rides for large group enrollees include an out-of-network charge for ambulance-related services that may put people at risk of getting surprise bills.
Taken together, as many as 1.5 million privately insured patients who are brought to an emergency room by an ambulance may be at risk of getting a surprise medical bill each year.
Where there is state or local regulation of ground ambulance billing practices, those laws may protect only certain types of ground ambulance rides. State laws protecting patients from surprise out-of-network ground ambulance bills do not apply to self-insured health plans.
The No Surprises Act requires the federal government to convene an advisory committee of federal and state officials, emergency medical services providers, and consumer representatives.
The advisory committee will provide recommendations on ways to protect consumers from surprise bills for ground ambulances. The advisory committee will also review ground ambulance charges and fees to recommend health insurance payment practices to prevent ground ambulance balance billing. Further federal or state legislative action would most likely be needed to implement the advisory committee recommendations.
The regulation and delivery of ground ambulance services could present complexities beyond those involved in preventing other surprise medical bills. Yet, from the perspective of patients, ambulance rides are exactly the kinds of situations where they feel powerless to avoid surprise bills.
Methods
NHAMCS is a national probability survey of visits to hospital emergency departments. Using 2018 NHAMCS, we estimated the number of emergency department arrivals by ambulance for those younger than 65 with private insurance (‘paytyper’ variable equals “Private Insurance”). For more information on NHAMSC, see here. One limitation is that a portion of these ambulance arrivals may include air ambulances, which are included in the surprise billing protections in the No Surprises Act. In addition, NHAMCS only includes ambulance rides which arrived at an emergency department.
To assess ground ambulance ownership status, we evaluated the NEMSIS data. We included events with a ground ambulance, service in response to a 911 call, patient treated and transport by EMS, and a destination to a free-standing or hospital emergency room. Among these events, we calculated the share of ground ambulance rides by the organization ownership type.
For the analysis of share of ground ambulance claims for large employer plans that included out-of-network charges for ambulance related-services, we analyzed a sample of medical claims obtained from the 2018 IBM Health Analytics MarketScan Commercial Claims and Encounters Database, which contains claims information provided by large employer plans. We only included claims for people under the age of 65. This analysis used claims for 18 million people representing about 22% of the 82 million people in the large group market. Weights were applied to match counts in the Current Population Survey for enrollees at firms of a thousand or more workers by sex, age, state and whether the enrollee was a policy holder or dependent. Weights were trimmed at eight times the interquartile range.
We identified days in which an enrollee had either an emergency or non-emergency ambulance ride with one of the following HCPCS codes:
- A0426 Ambulance service, advanced life support, non-emergency transport
- A0427 Ambulance service, advanced life support, emergency transport
- A0428 Ambulance service, basic life support, non-emergency transport
- A0429 Ambulance service, basic life support, emergency transport
We excluded days that included an air ambulance charge. We then identified the share of ambulance rides with at least one out-of-network charge for ambulance-related services (which includes the following HCPCS codes: A0021, A0380, A0382, A0384, A0390, A0392, A0394, A0396, A0398, A0420, A0422, A0424, A0425, A0426, A0427, A0428, A0429, A0432, A0433, A0434, A0888, A0999). We did not include other out-of-network charges that may happen on the day (e.g., emergency department or in-patient hospital charges). The classification as an emergency or non-emergency ride depends on the HCPCS code and not whether the ride concluded at an emergency department. In our analysis, 70% of emergency and 19% of non-emergency ground ambulance rides had an emergency room visit on the same day.
The Peterson Center on Healthcare and KFF are partnering to monitor how well the U.S. healthcare system is performing in terms of quality and cost.