Despite spending more money per capita on healthcare than any similarly large and wealthy nation, the United States has a lower life expectancy than peer nations and has seen worsening health outcomes since the onset of the COVID-19 pandemic.
This chart collection combines various measures of quality of care in the United States and other large, high-income nations to show how the U.S. stacks up against its peers and how that has changed over time. While inconsistent and imperfect metrics make it difficult to firmly assess system-wide health quality, measures of long-term health outcomes, treatment outcomes, patient safety, and patient experiences suggest the U.S. health system provides lower-quality care than its peers. The U.S. performs worse in long-term health outcomes measures (such as life expectancy), certain treatment outcomes (such as maternal mortality and congestive heart failure hospital admissions), some patient safety measures (such as obstetric trauma with instrument and medication or treatment errors), and patient experiences of not getting care due to cost. The U.S. performs similarly to or better than peer nations in other measures of treatment outcomes (such as mortality rates within 30 days of acute hospital treatment) and patient safety (such as rates of post–operative sepsis).
Long-Term Health Outcomes
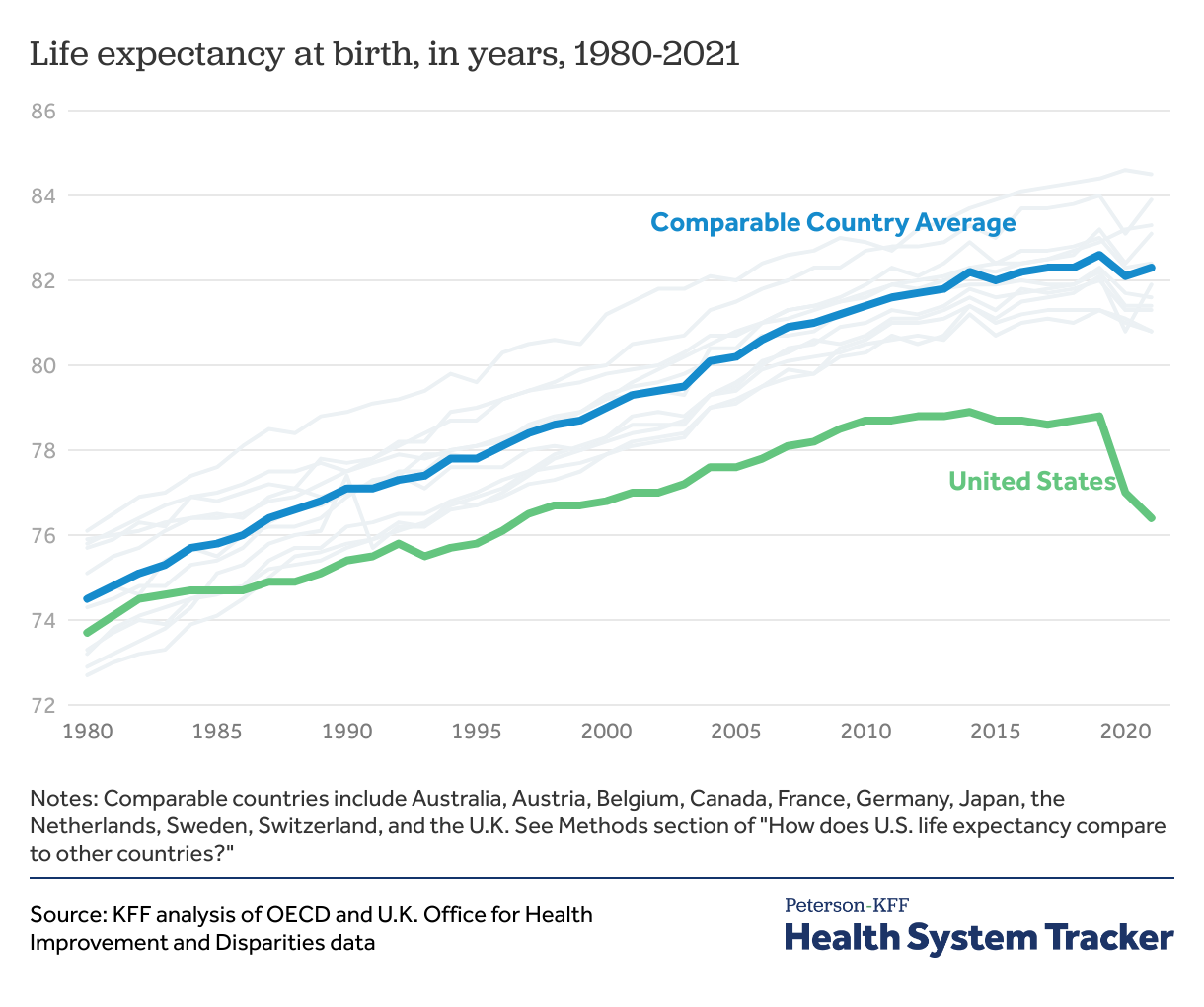
Life expectancy continued to drop in the U.S. in 2021 while rebounding in most peer countries
As discussed in more detail in a separate brief, life expectancy at birth was similar in the U.S. and peer countries on average in 1980 (73.7 and 74.5 years, respectively), but the gap has grown substantially in the following decades, as peer nations saw more rapid improvement in life expectancy than the U.S. The COVID-19 pandemic further widened this gap, and life expectancy in 2021 was 6 years shorter in the U.S. than in peer countries (76.4 years in the U.S. and averaged 82.3 years in comparable countries, on average).
The above data are period life expectancy estimates, based on excess mortality observed in each year. The period life expectancy at birth represents the mortality experience of a hypothetical cohort if current conditions persisted into the future, not the mortality experience of a birth cohort.
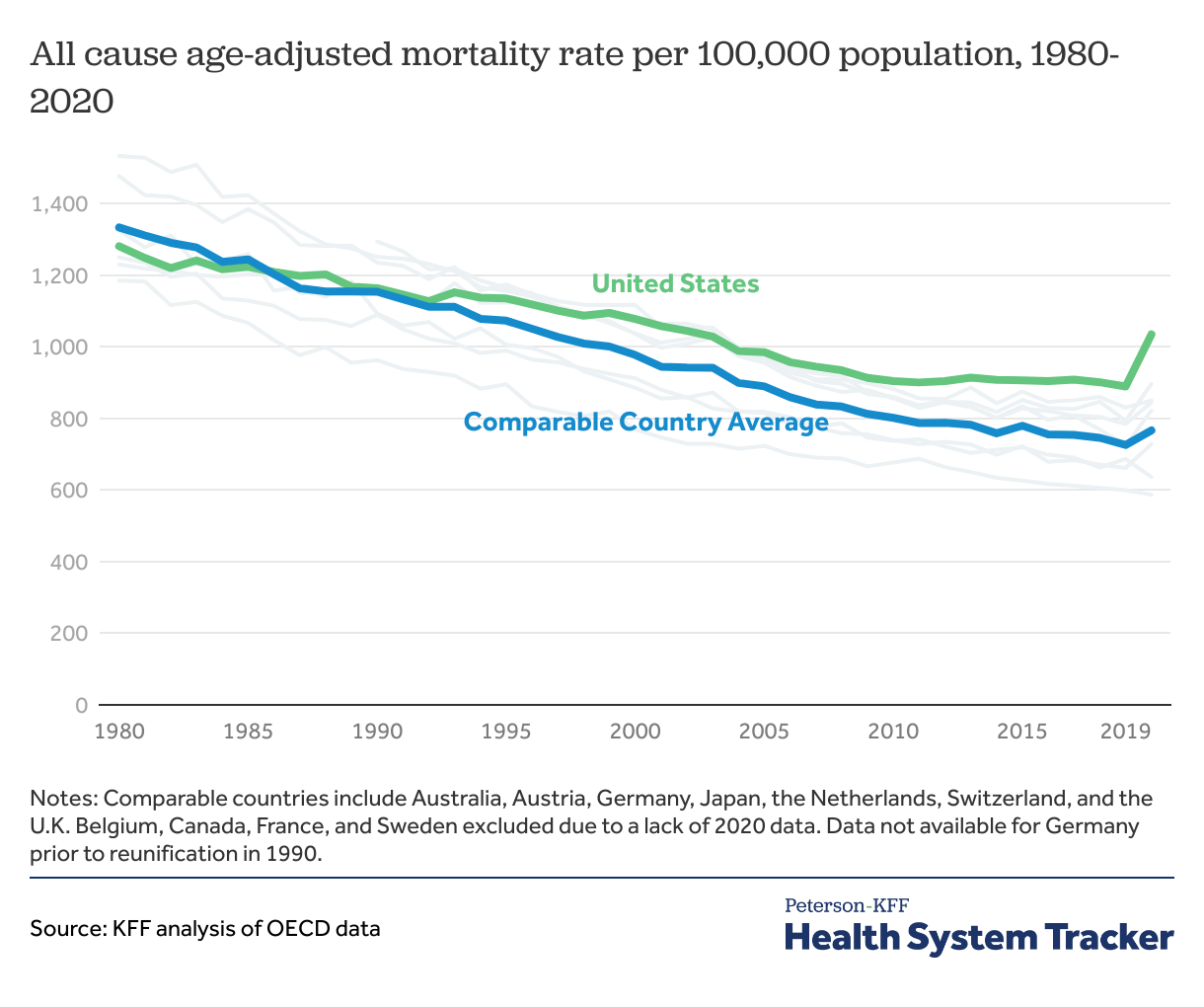
Since the pandemic, the gap in mortality rates between the U.S. and comparable countries has widened
All-cause mortality rates — the number of deaths per 100,000 people, adjusted for age differences across countries — plateaued in the U.S. in the 2010s, while continuing to fall in other peer nations. From 1980 to 2020 (the latest year with comparable data), the overall mortality rate from all causes of death in the U.S. fell by about 19%, compared to a 43% decline in peer countries.
The COVID-19 pandemic resulted in increased mortality across most nations, though the U.S. saw a significantly higher increase than many other countries. The gap in mortality rates between the United States and peer nations was at its highest point in 2020.
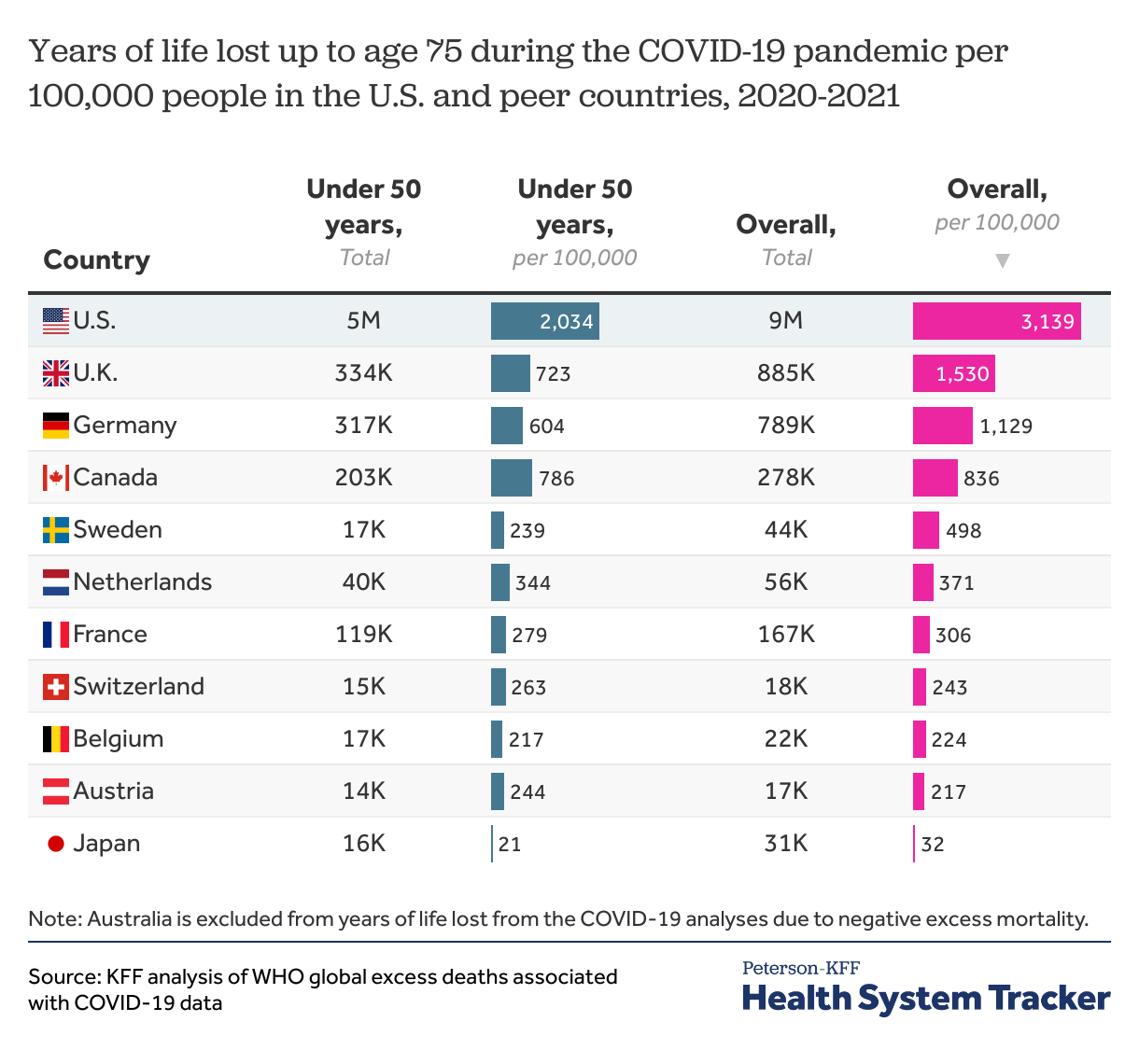
Premature death rates in the U.S. continue to be higher than in comparable countries
In addition to overall mortality rates, the “years of life lost” metric marks the extent of premature deaths within a population by providing more weight to deaths at younger ages. The U.S. and comparable OECD countries have made progress in reducing years of life lost from 1990 to 2019 (down 24% and 42%, respectively), although the gap between the U.S. and comparable countries has increased over time.
The U.S. had the highest increase in premature deaths due the pandemic in 2020 and 2021. The per capita premature excess death rate in the U.S. was over twice as high as the next closest peer country, the U.K. The higher rate of new premature deaths in the U.S. compared to peer countries was driven in part by racial disparities within the U.S. The premature excess death rates for American Indian and Alaska Native, Black, Hispanic, and Native Hawaiian and other Pacific Islander populations in the U.S. were 3 times higher than the rates among White or Asian populations. The U.S. health system consistently results in higher rates of mortality and premature deaths among people of color.
Children and teens in the U.S. are less likely to make it to adulthood than in peer countries, with the U.S having higher rates of motor vehicle accidents, firearm deaths, and suicide deaths among children and teens.
Disease burden, which accounts for both premature death and years living with disability, is often measured using disability adjusted life years (DALYs). As of 2019 — the most recent year with available data — DALYs have declined in the U.S. and comparable countries since 2000, though the U.S. continued to have higher age-adjusted disease burden rates than peer countries. In 2019, the DALY rate was 37% higher in the U.S. than in comparable countries, on average.
Treatment Outcomes
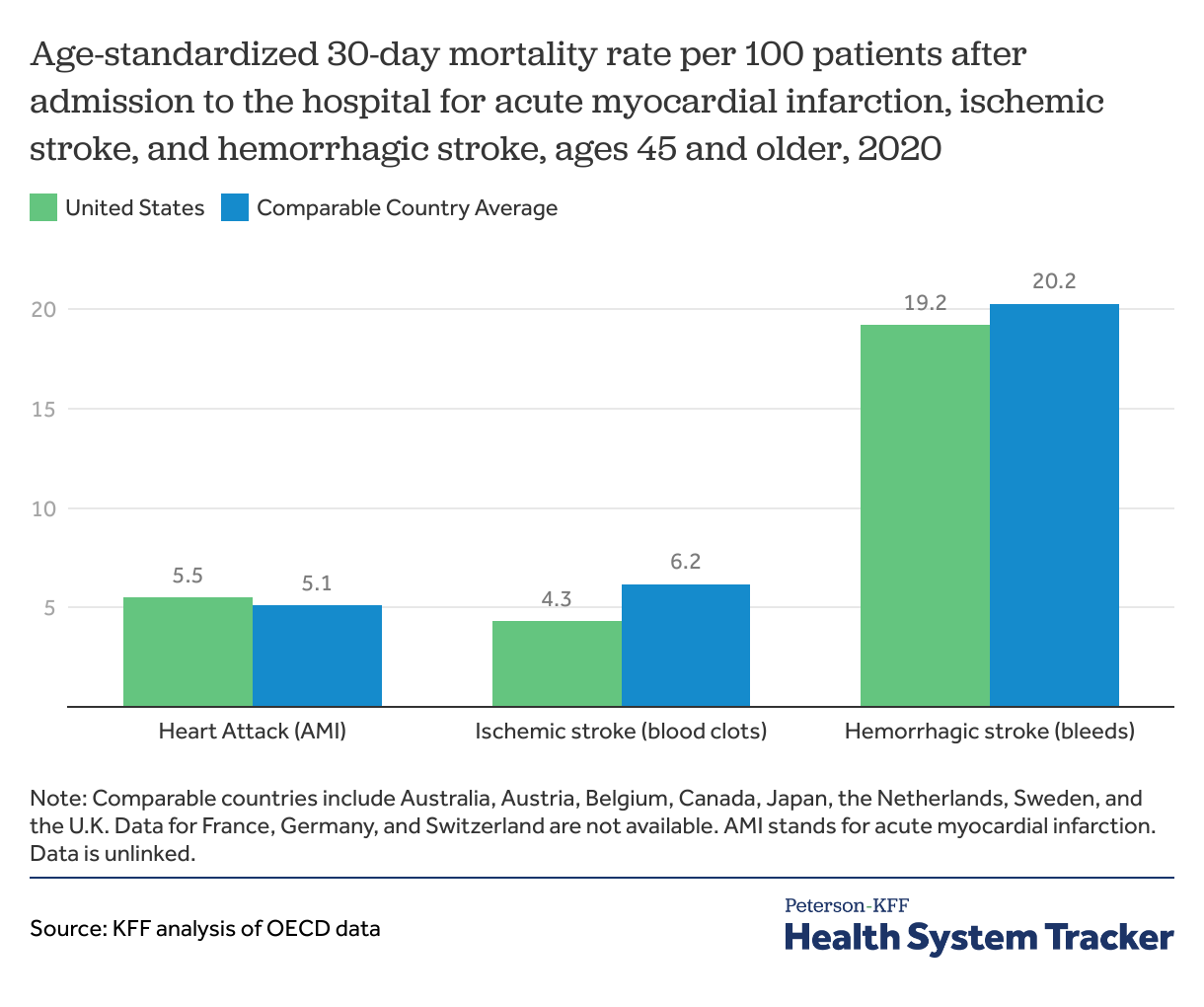
30-day mortality for strokes is lower in the U.S. than in comparable countries, on average
Mortality within 30 days of being admitted to a hospital is not entirely preventable, but high quality of care can reduce the mortality rate for certain diagnoses. The 30-day mortality rates after hospital admissions for heart attacks (acute myocardial infarction) and hemorrhagic stroke (caused by bleeding) are similar in the U.S. and comparable countries average. The 30-day mortality rates for ischemic strokes (caused by blood clots) was 4.3 deaths per 100 patients in the U.S. in 2020, compared to an average of 6.2 deaths per 100 patients in similar countries. While the U.S. has lower rates of mortality due to these conditions than the average across peer nations, it is important to note that several peer nations have lower rates than the U.S.
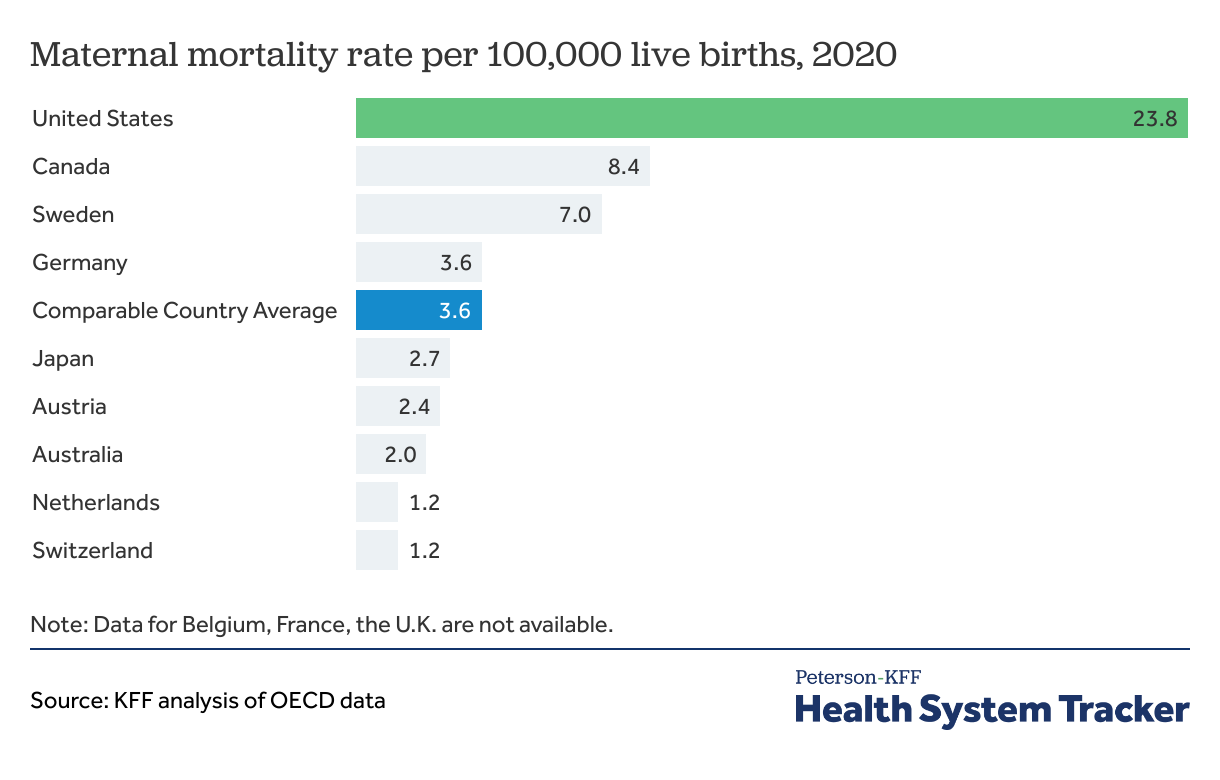
Maternal mortality rates in the U.S. have risen over time and are much higher than in peer countries
While wealth and economic prosperity are highly correlated with lower maternal mortality rates, the U.S. is an outlier with the highest rate of pregnancy-related deaths (23.8 deaths per 100,000 live births in 2020) when compared to similar countries (3.6 deaths per 100,000 live births).
Within the U.S., there are significant racial disparities in maternal mortality rates. The maternal mortality rate for Black mothers is about 3 times the rate for White mothers — a disparity that persists across age and socioeconomic groups. Every race and ethnicity, socioeconomic, and age group in the United States sees higher maternal mortality rates than the average in comparable countries. Maternal mortality in the U.S. has risen in recent years, sparking concern from the medical community and regulators.
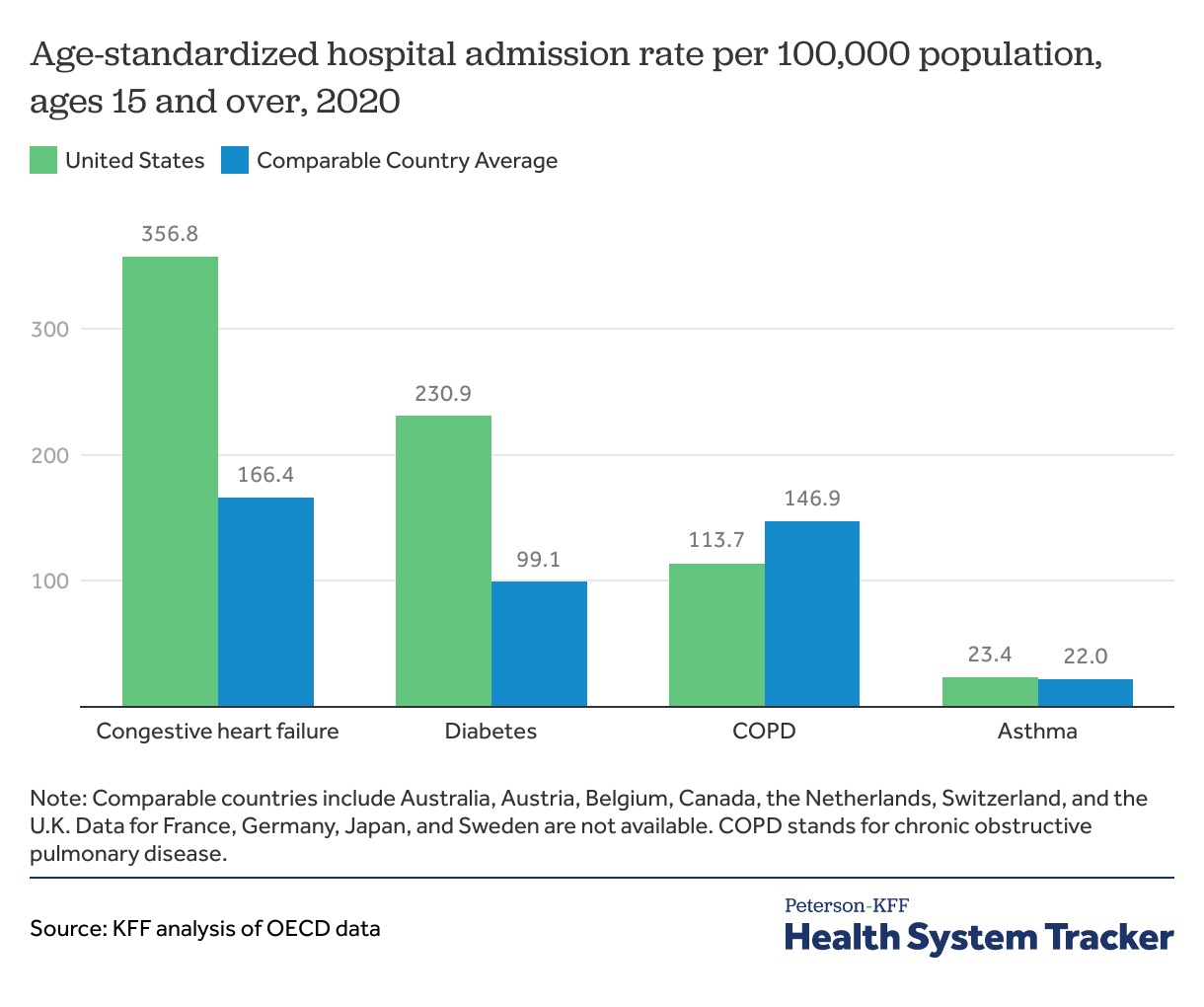
Hospital admissions for diabetes and congestive heart failure were more frequent in the U.S. than average across comparable countries
Hospital admissions for certain chronic diseases, such as cardiac conditions, chronic obstructive pulmonary diseases (COPD), asthma, and diabetes, can arise for a variety of reasons, but preventive services — or lack thereof — play a large role. Hospital admission rates in the U.S. are higher than in comparable countries for congestive heart failure and complications due to diabetes, and some admissions for these chronic conditions could be minimized with adequate primary care. Admission rates in 2020 are likely impacted by the COVID-19 pandemic — patients were less likely to seek hospital treatment, and hospitals were at times overwhelmed and unable to admit patients who would have been admitted in a different year.
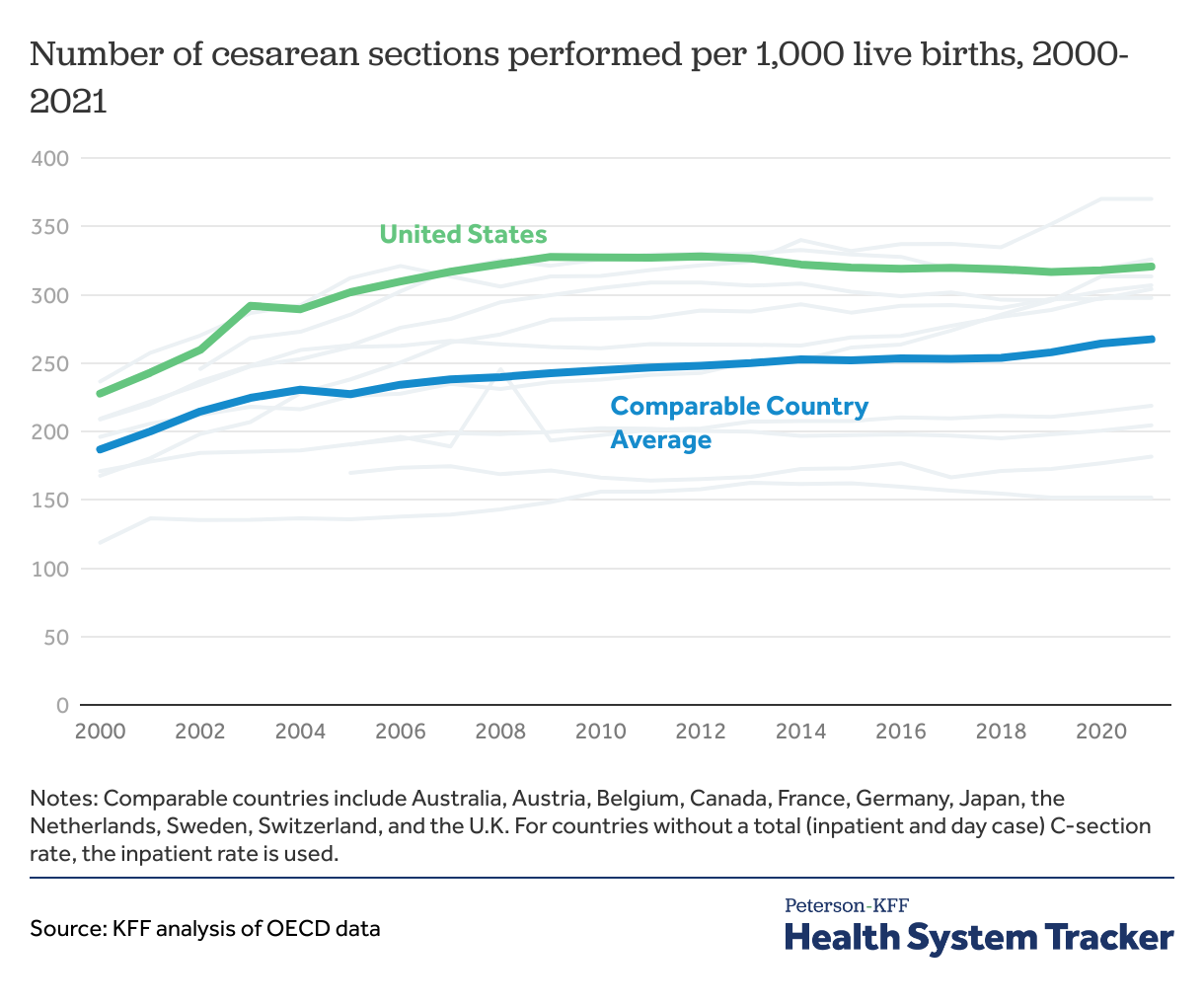
More cesarean sections are performed in the U.S. than in comparable countries
Cesarean sections are one of the most commonly performed surgical procedures in the U.S. and have become a key indicator of quality of care in maternal health. Cesarean sections can be lifesaving — however, when they are not medically indicated, they can pose unnecessary risks for mothers, including an increased chance of blood clots, infections, and other complications that require further surgery.
The U.S. has consistently had higher cesarean section rates than most of its peers, though rates have decreased slightly in recent years. In 2021, the rate of cesarean sections per 1,000 live births was 321 in the U.S. and an average of 267 in comparable countries.
Patient Safety
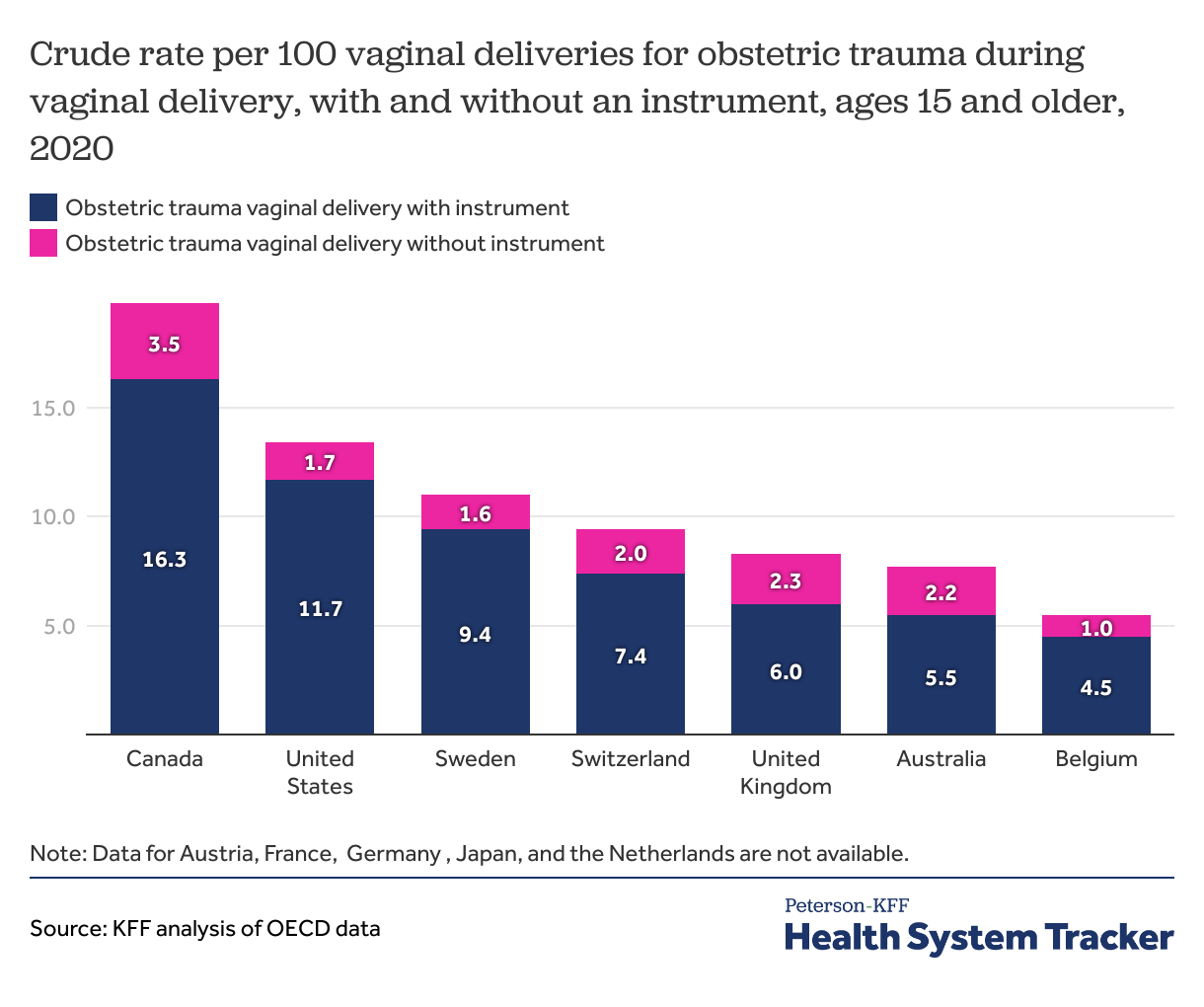
Obstetric trauma during vaginal delivery is more common in the U.S. than in most comparable countries, especially when instruments are involved
Obstetric trauma is more likely to occur in deliveries where instruments are utilized (i.e., forceps). The rate of obstetric trauma during deliveries with an instrument in the U.S. was 11.7 per 100 vaginal deliveries in 2020, higher than most comparable countries with available data. The rate of obstetric trauma during deliveries without an instrument in the U.S. was 1.7 per 100 vaginal deliveries in 2020, on the lower end among comparable countries with available data.
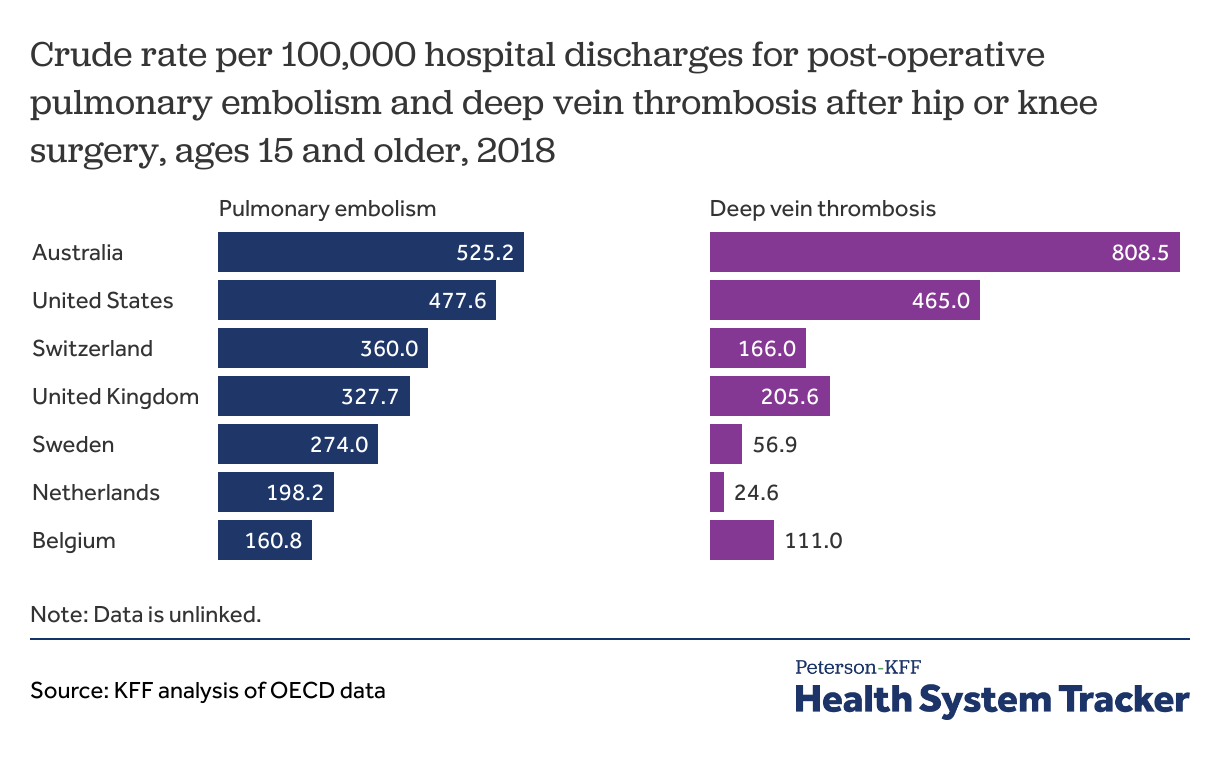
Post-operative complications — such as pulmonary embolism or deep vein thrombosis — are more common in the U.S. than most peer countries
Rates of post-operative complications are an important measure of hospital safety. Pulmonary embolisms and deep vein thrombosis are common complications after major surgeries, such as hip or knee replacement. The prevalence of post-operative clots for these procedures is higher in the U.S. than in the U.K., Sweden, Belgium, and the Netherlands, but lower than in Australia.
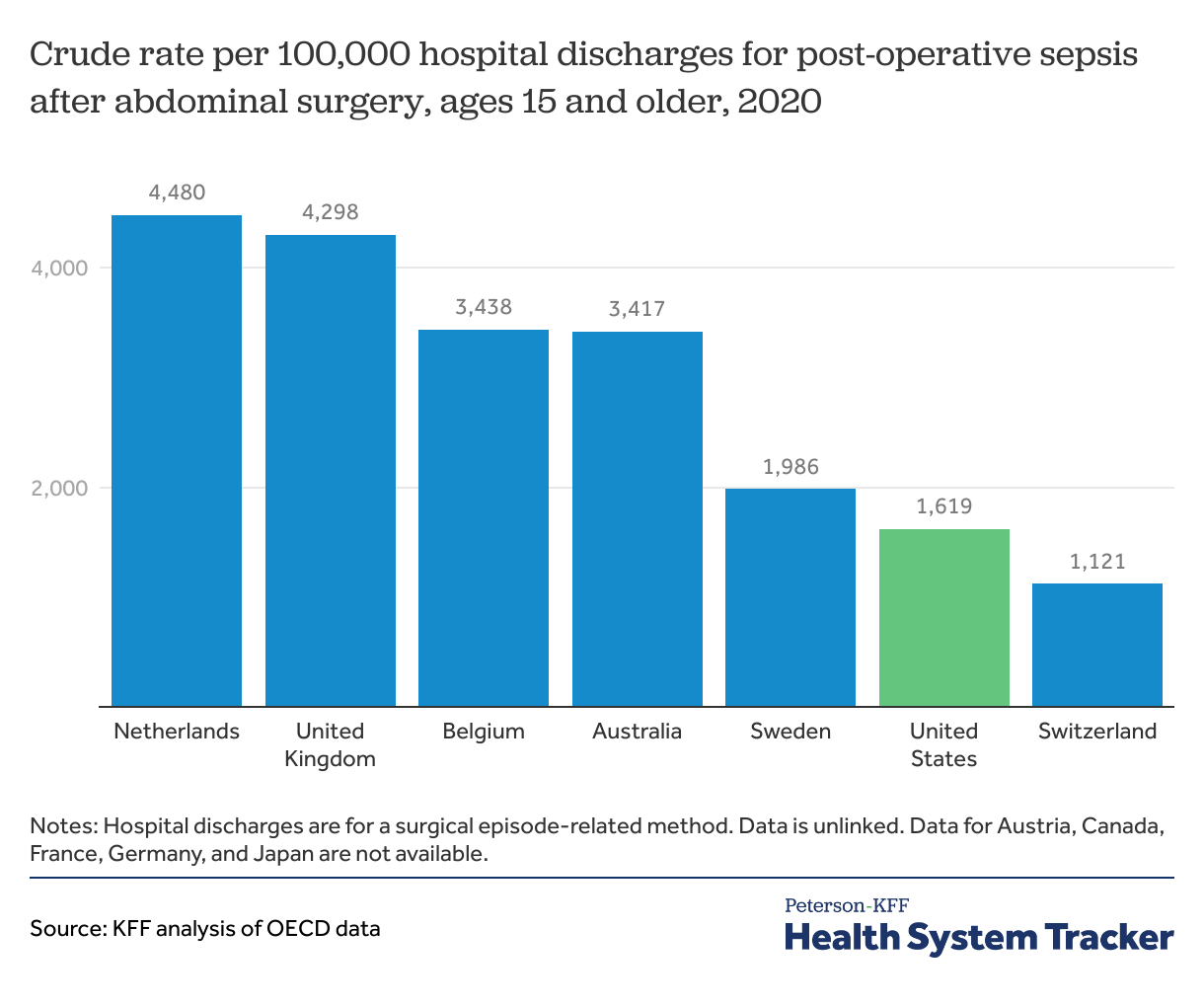
Post-operative sepsis is less common in the U.S. than in most peer countries
Sepsis is a serious complication for patients with infections, and effects can range from organ failure and shock to death in severe cases. Rates of post-operative infections and sepsis are an important marker of care quality for patients undergoing surgery, because this is a major source of morbidity and mortality that can sometimes be prevented. Prevention is multifactorial and can involve proper operative techniques and training, hygiene and safety protocols, and antibiotic utilization, amongst other things. The rate of post-operative sepsis following abdominal surgery is just under 2% in the U.S., lower than in most peer countries that report data.
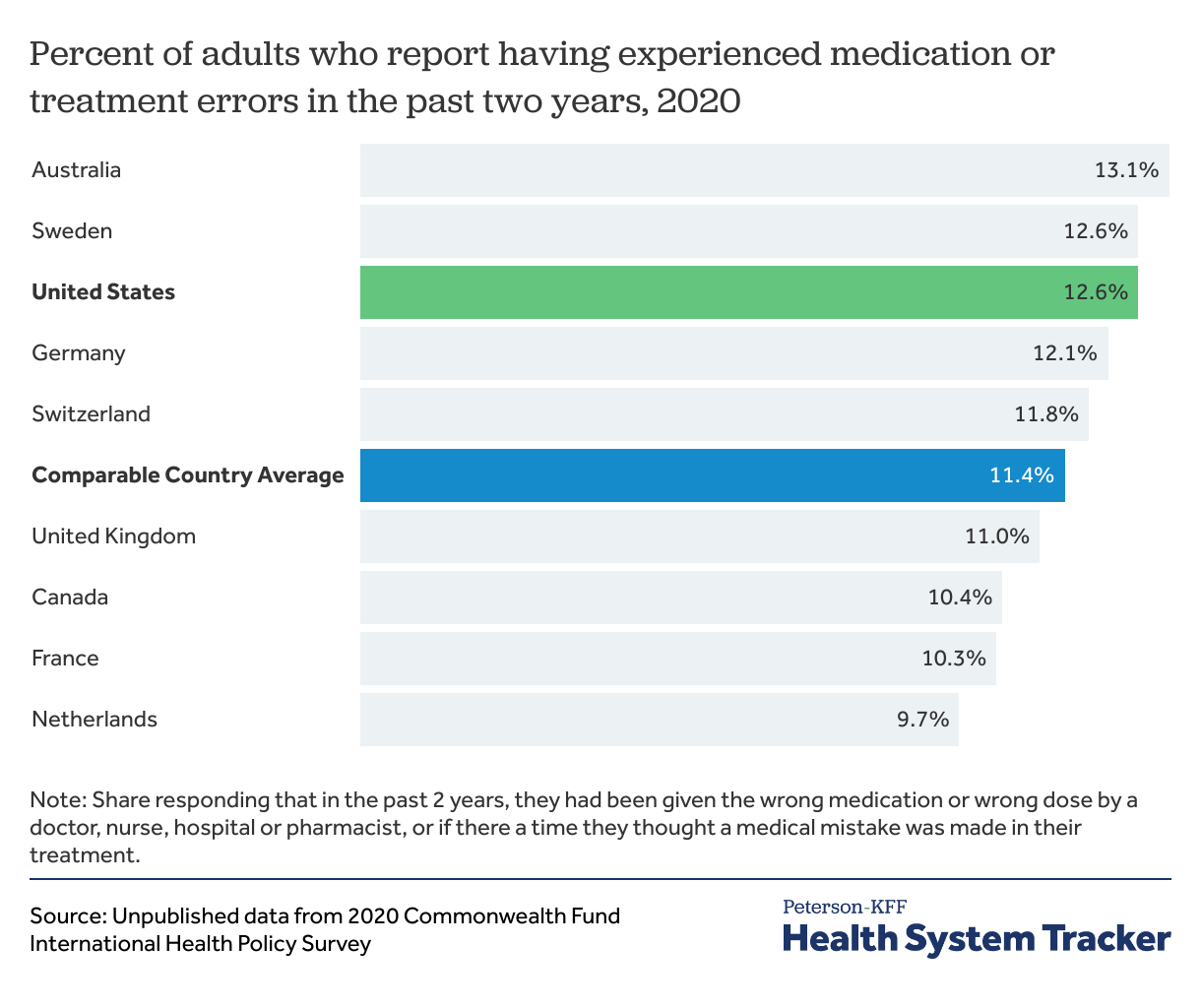
The U.S. has higher rates of reported medication and treatment errors than most comparable countries
Patients in the U.S. are more likely than those in comparable countries to report experiencing a medication or medical error at some point during their care, according to a survey by the Commonwealth Fund. In this case, medication errors include being given the wrong medication or dose, and treatment errors indicate that people thought a medical mistake had been made in their treatment or care. In 2020, 12.6% of patients in the U.S. experienced a medical error compared to 11.4% of patients in similar countries.
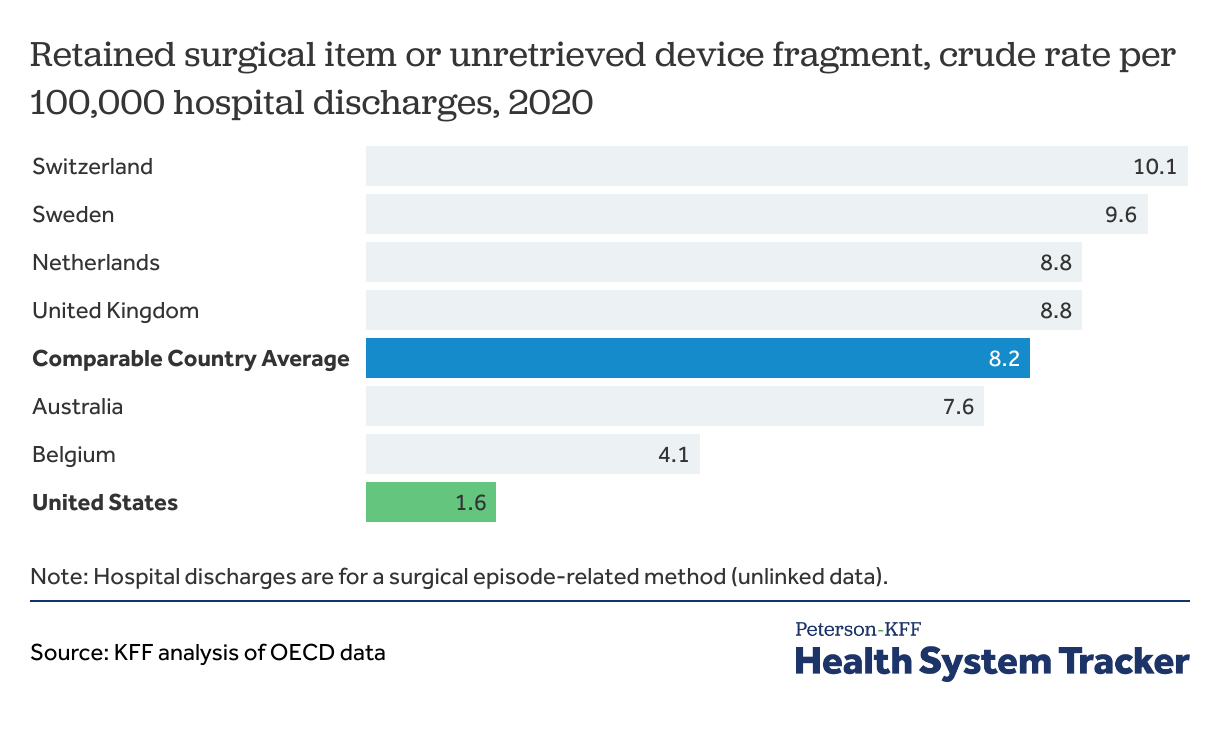
Among peer countries, the U.S. had the lowest rate of retained surgical item or unretrieved device fragments in 2020
Unintentionally retained items or device fragments following surgical procedures can result in pain, infection and even life-threatening consequences for patients. The U.S. has the lowest rate of retained surgical items or unretrieved device fragments in 2020, at 1.6 per 100,000 surgical hospital discharges, compared to an average rate of 8.2 per 100,000 surgical hospital discharges in comparable countries.
Patient Experiences
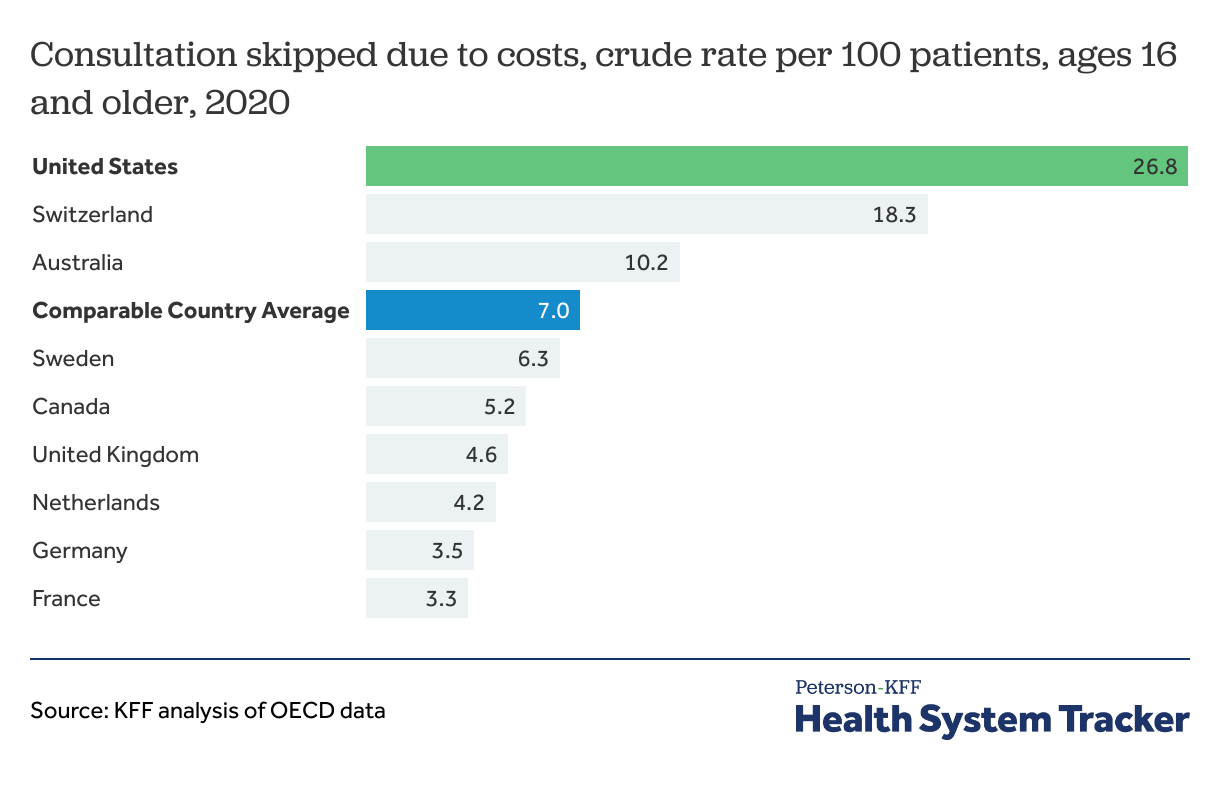
The U.S. has higher rates of consultations missed due to costs than comparable countries in 2020
Patients in the U.S. are more likely to experience missed consultations with their provider due to costs. In 2020, the rate of consultations missed due to costs in the U.S. was 26.8 per 100 patients, compared to 7.0 per 100 patients on average in comparable nations for the same year. When patients choose not to meet with their physicians due to cost or any other reason, it can lead to worse health outcomes and more expensive care needed at later points in the patient’s life.
Discussion
There are limited comparable measures of quality available. Among measures we can compare, the U.S. performs similarly or better than its peers for when intensive, acute care is required, such as for 30-day mortality after heart attack or stroke admissions. However, for long-term health measures and conditions where care coordination or public health efforts may improve outcomes (for example, maternal outcomes or chronic condition hospitalization rates), the U.S. consistently falls short. Of particular concern, outcomes measures such as all-cause mortality, maternal mortality, and years of life lost have stagnated or worsened in the U.S. in recent years, even as peer nations have seen improvement in these metrics.
Throughout this chart collection, measures such as long-term health outcomes, treatment outcomes, patient safety, and patient experiences are used as a proxy to analyze the quality of health systems in the U.S. and 11 other countries identified as similarly wealthy based on total GDP and GDP per capita. While these indicators allow for cross-country comparisons, they do not necessarily provide a comprehensive overview of the quality of each country’s respective health system. Additional indicators can be used to provide further insight into the quality of countries’ health systems. However, country specific differences in population health, payment systems, survey metrics/methods, and demographics present barriers to cross country comparisons.
Methods
Most data used here are sourced from the Organization for Economic Co-operation and Development (OECD), which compiles health quality statistics and data from member nations.
All cause age-adjusted mortality data was interpolated for the U.K. in 2000 and Australia in 2005 due to unavailable data.
C-section data is not available for Belgium and Sweden from 2000-2004, Switzerland from 2000-2001, Belgium from 2015 and the Netherlands from 2011 and 2020; 2021 data is not yet available for Australia, Canada, the Netherlands and the United Kingdom. Data points are interpolated for the comparable country average in those years.